Definition: What is stomatitis?
Stomatitis is an umbrella term for various inflammations of the oral mucosa, which are often painful. This technical term has its origins in Greek: "stoma" means mouth and "itis" is the syllable used in medical language for inflammation.
The oral mucosa covers our entire mouth: the cheeks, throat, palate and also the inside of the lips. Gums are also made up of mucous membrane. However, inflammation of the gums is not technically known as stomatitis. The correct term for this is gingivitis.
When the oral mucosa is healthy, it has a pink colour. However, inflammation often leads to redness, swelling, burning pain and ulcers. A whitish coating or whitish patches may also appear. Inflammation of the oral mucosa can occur in a single area or even over a large area - depending on the type of stomatitis. As a rule, inflammation of the oral mucosa heals within one to two weeks.
Stomatitis can - if it is the main symptom - be a disease in its own right, but it can also be a concomitant symptom of another disease or even a side effect of treatment.
Causes: Different types of stomatitis
There are many causes of inflammation of the oral mucosa. Several factors can also interact. Stomatitis can be triggered by an infection - in which case it is also contagious - or caused by injury or irritation.
Bacteria
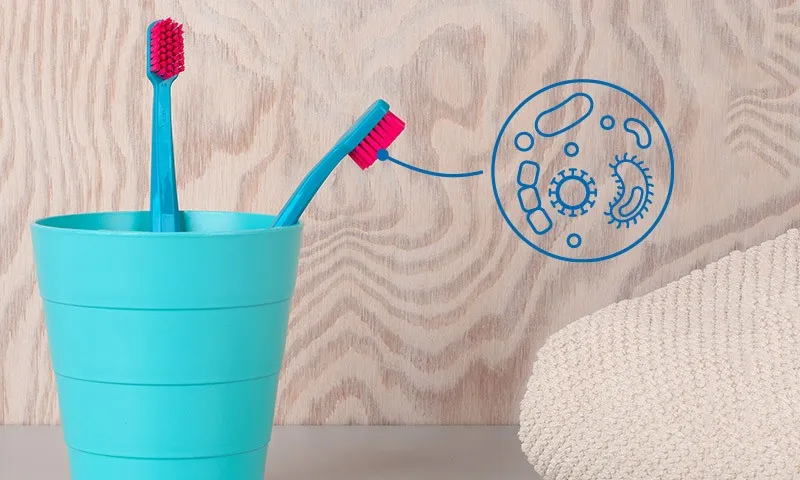
Our mouths are teeming with bacteria. This is normal and should be the case: after all, many bacteria are "good" and even helpful for the human organism. However, if the balance is upset and harmful bacteria multiply undisturbed, inflammation can occur. This can be caused by poor oral hygiene or pre-existing gum disease - for example gingivitis or periodontitis. Bacteria can also attach to dentures - for example implants. This is referred to as peri-implant mucositis. Inflammation can then spread from the gums to other areas of the oral mucosa.
A particularly severe form of bacterial inflammation of the oral mucosa is "ulcerative stomatitis". This is a bacterial infection in which purulent ulcers often form. The terms "ulcerative" or "ulcerative" describe these ulcers or deep tissue damage. This form of stomatitis can occur with infectious diseases, chronic poisoning or a lack of white blood cells.
Good to know:
Did you know that harmless gum inflammation can turn into serious periodontitis? You can find out how to get rid of gum inflammation quickly here:
Viral infection
When stomatitis is triggered by an initial infection with herpes viruses, doctors refer to it as "stomatitis aphthosa" or "stomatitis herpetica". Children under the age of five and people with a weakened immune system in particular can react with severe inflammatory symptoms: Painful blisters and small ulcers often form in the entire mouth area. The gums are swollen and tend to bleed. The pathogen that causes this disease, colloquially known as "mouth sores", is the herpes simplex virus type 1, which is also responsible for cold sores.
Beware of confusion: The term "stomatitis aphthosa" is also used for inflammations in which aphthae form on the oral mucosa - more on this in the next section.
Good to know:
The Coxsackie virus can also lead to inflammation of the oral mucosa. Here too, children are primarily affected. However, the blisters in this viral infection are not limited to the mouth area, but also appear on the hands and feet. This is why it is also referred to as hand-foot-mouth disease.
Aphthae
Aphthae are one of the most common inflammations of the oral mucosa. Initially, the oral mucosa burns and itches, followed by whitish-reddish inflammation spots that can appear anywhere on the oral mucosa. Although they cause pain, they are not dangerous and heal on their own. If people get aphthae again and again, they are referred to as "chronic recurrent aphthae". The interval between the occurrence of aphthae can vary greatly: Some people only have a short break of a few weeks, while for others it takes months or even years before the next aphthous ulcer occurs. It is not yet clear why aphthae form.
You can find out more about aphthae in our article:
Mushrooms
When stomatitis is caused by fungi - usually Candida albicans - it is referred to as oral thrush or oral candidiasis. Those affected report a furry feeling in the mouth and a white coating on the oral mucosa. There are often sores under the wipeable coating that bleed quickly. In people with a strong immune defence, the presence of these fungi in the mouth does not lead to inflammation of the oral mucosa. However, if the immune system is weakened - for example due to chemotherapy or HIV infection - or if the "good" bacteria have been killed off by taking antibiotics, fungi can become prevalent. Babies are also susceptible to this because their mucous membranes are not yet colonised with healthy germs.
You can find out more about oral thrush and the treatment options here:
Injuries and irritations
Inflammation, pain and swelling can also occur after extensive dental treatment in which the gums have been injured - such as after a wisdom tooth operation. Other injuries can also make it easier for "bad" bacteria to settle in the oral mucosa. These include, for example, an accidental bite on the cheek, an ill-fitting denture, but also a sharp tooth edge.
Certain substances - especially nicotine and alcohol - are also bad for the oral mucosa and can cause inflammation. You should also be careful with very hot or very acidic foods. A burn or scald can also damage the oral mucosa and possibly trigger stomatitis. Toothpastes containing sodium lauryl sulphate (SLS) are also suspected of irritating the oral mucosa. You should therefore make sure you avoid this ingredient when buying your toothpaste.
Good to know:
The toothpaste varieties from Curaprox are all free from harmful ingredients such as sodium lauryl sulphate (SLS), microplastics, triclosan etc. and protect your teeth and oral flora with natural enzymes.
Allergies
Allergies to certain foods or medications can also lead to inflammation of the oral mucosa. In the medical world, this is referred to as "allergic stomatitis". This can lead to redness, swelling and itching. Blisters or ulcers are less common.
Vitamin deficiency
A lack of certain vitamins (A, B or C) as well as iron and folic acid can also be responsible for stomatitis.
Diseases
Stomatitis can also be a side effect of other diseases: diabetics, for example, have an increased risk of oral mucosal inflammation because their immune system is weakened and the body is therefore less able to fight inflammation. Saliva production can also decrease with diabetes, which has a negative impact on oral health. The same also applies to Corona: Dry mouth and inflammation of the oral mucosa are among the most common oral symptoms of the Covid-19 virus.
Saliva protects teeth and mucous membranes from harmful bacteria. Bacteria can spread much more easily in a dry mouth. Chronic inflammatory bowel diseases (e.g. Crohn's disease, ulcerative colitis and coeliac disease), as well as blood, metabolic or skin diseases, can also cause inflammation of the oral mucosa.
Stress
The human immune system is weakened by constant stress. As a weak immune system offers poorer protection against bacteria, viruses and fungi, people who are frequently exposed to stress suffer more frequently from aphthae and other inflammations of the oral mucosa.
Pregnancy
During pregnancy, the tissue throughout the body loosens - including in the mouth. This makes it particularly easy for bacteria to penetrate the gums and oral mucosa. This is why many pregnant women also complain of gum inflammation. As you already know, gingivitis can also spread to other parts of the oral mucosa. Menopause can also lead to increased inflammation of the oral mucosa due to hormonal changes.
Good to know:
Find out here why you should brush your teeth particularly well during pregnancy and how you can prevent damage:
Cancer treatment
Inflammation of the oral mucosa is very common in cancer patients: around 60 per cent of people who receive chemotherapy suffer from inflammation of the oral mucosa. People who receive radiotherapy in the head and neck area also frequently suffer from severe inflammation of the oral mucosa. In severe cases, those affected have to be artificially fed for a certain period of time because the inflammation makes it impossible to eat. This acute form of stomatitis is also referred to as mucositis.
Find out what else you need to know about dental health and cancer treatment here:
How to protect your teeth from the side effects of chemotherapy and radiotherapy
Oral cavity cancer
If an ulcer on the oral mucosa does not disappear over a longer period of time, it may not be a harmless inflammation but could be something more serious. In this case, be sure to have it examined by a doctor. Oral cancer can occur anywhere in the mouth. If the oral mucosa is affected, it is referred to as squamous cell carcinoma. If tumours in the oral cavity are detected early, the prognosis is good.
Good to know:
In our article, you can find out exactly how oral cavity cancer is recognised, what the chances of recovery are and what exactly the treatment looks like:
Symptoms: How does stomatitis manifest itself?
Depending on what has caused the oral mucosal inflammation, different symptoms can occur on the palate, throat, inside of the cheeks and inside of the lips, some of which can also extend to the tongue. For example, inflammation of the oral mucosa caused by a fungal infection often results in a white coating on the cheeks and tongue. A herpes infection, on the other hand, often leads to the formation of blisters throughout the mouth.
Common symptoms and accompanying symptoms include
- Redness
- Swelling
- Burning
- Itching
- Pain (especially when eating and drinking)
- Bleeding
- White coating (oral thrush)
- Blisters, swelling of the lymph nodes, fever (initial infection with herpes viruses)
- Bad breath
- Dry mouth
- Open sores or small ulcers
- Purulent ulcers (ulcerative stomatitis)
- Aphthae
Good to know:
Bad breath is very troublesome for many people. You can find out how to keep your breath fresh in our article:
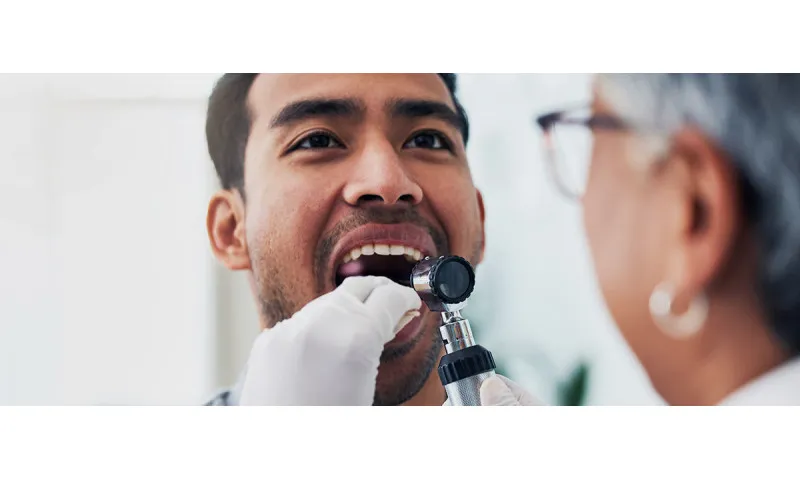
Diagnosis: Which doctor should I see for stomatitis?
You already know that inflammation of the oral mucosa can have various causes. Accordingly, there are also differences in treatment. So that you can treat your stomatitis effectively, you should have the change in the oral mucosa examined by a doctor. If necessary, he or she will also take a swab so that a laboratory can determine whether the inflammation is an infection and, if so, which pathogen is responsible.
But which doctor is actually responsible for the oral mucosa? You can choose between a dentist, family doctor or dermatologist.
Treatment: What to do with stomatitis?
Simple inflammation of the oral mucosa and aphthae often disappear on their own without you having to treat them. However, if there is an underlying infection, special medication can help. You can also alleviate inflammation of the oral mucosa to some extent with home remedies. You can find out which therapeutic measures are suitable here:
Medication for inflammation of the oral mucosa
If your oral mucositis is caused by an infection, medication can help: Antifungals kill fungi, antibiotics work for bacterial infections and antivirals can help with viral infections.
If the cause is unclear, only the symptoms can be treated. Anaesthetics such as lidocaine can reduce the perception of pain and can be applied directly to the affected area as an ointment or gel. Medication with anti-inflammatory agents can also be used to prevent the inflammation from spreading further. Astringent tinctures based on myrrh or rhubarb root contract the tissue of the oral mucosa and have a pain-relieving, antibacterial effect.
Mouthwashes with antiseptic agents such as chlorhexidine can kill germs. However, you should seek advice from your dentist on how long and how often you should use such mouthwashes. Continuous use is not necessary and may even be harmful. Antibacterial mouthwashes not only kill the "bad" bacteria that cause inflammation, but also the "good" bacteria and therefore harm the microbiome in the mouth.
You can also buy homeopathic remedies such as Schüssler salts or globules for oral mucosal inflammation at the pharmacy. However, you should note that there is no scientific proof of the effectiveness of such remedies.
Good to know:
In addition to chlorhexidine, the products in the Perio plus range from Curaprox also contain Citrox®, a natural extract from bitter orange, which has an antibacterial and antioxidant effect and prevents the formation of dental plaque.
Home remedies for inflammation of the oral mucosa
The home remedy of choice for treating oral mucosal inflammation is mouthwashes with herbal teas, which you can use several times a day. Make sure that the tea has cooled down sufficiently before you rinse your mouth with it to prevent scalding.
The following teas can help:
- Camomile tea has a pain-relieving, anti-inflammatory and antibacterial effect.
- Peppermint tea has a disinfectant effect.
- Mallow tea promotes healing, relieves pain and inhibits inflammation.
- Marigold tea has a disinfectant effect and boosts the body's defences.
- Sage tea has an antibacterial effect and protects against fungal infections.
- Thyme tea provides fresh breath, has an antibacterial effect and also protects against fungal infections.
Adapt your diet and lifestyle
While your oral mucosa is inflamed, you should avoid additional irritation as much as possible.
These include:
- Alcohol
- Tobacco
- Hard food
- Hot drinks
- Sour food
- Savoury dishes
- Hot dishes
- Carbonated drinks
Instead, you can temporarily eat light meals, i.e. soups, soft-cooked food (vegetables, fish or tender meat) or pureed food.
Brush your teeth anyway
If your oral mucosa is inflamed, it doesn't mean that you can stop brushing your teeth now. In fact, that would be counterproductive. After all, bacteria can multiply particularly easily in the mouth. Make sure you use a soft toothbrush.
Good to know:
Anyone who often has to deal with inflammation in the mouth is well advised to use a toothbrush with extra-soft bristles, such as the Velvet from Curaprox, which cleans very gently but effectively with 12460 filaments.
Preventing stomatitis: tips for healthy oral mucosa
If you've ever had an inflammation of the oral mucosa, you know how unpleasant it is. To minimise the risk of re-inflammation in the future, we have put together a few helpful tips for you:
1. Brush your teeth regularly
Proper dental care is the be-all and end-all for your oral health. If you brush your teeth twice a day for around three minutes and thoroughly remove plaque, you are doing your entire oral cavity a big favour. After all, we know that inflammation of the gums can also spread to other parts of the oral mucosa.
Good to know:
Do you already brush your teeth twice a day for three minutes? That's great! But are you doing it right? In our guide, we describe the - scientifically proven - most effective tooth brushing technique:
2. Use the right dental care products
The active ingredient SLS is suspected of causing irritation of the oral mucosa. Avoid toothpaste types that contain this active ingredient and instead opt for toothpaste with fluoride and natural active ingredients - for example 'Be you' toothpaste from Curaprox.
A toothbrush that is too hard and scrubs too hard can damage your gums. A soft toothbrush with a densely packed bristle head is much better. This applies not only if your oral mucosa is inflamed, but also for everyday brushing. The reason: a hard toothbrush not only causes damage, but cannot clean your teeth thoroughly because the bristles are not flexible enough.
3. Clean interdental spaces
Even if you brush your teeth thoroughly twice a day, you're not done with your dental care routine: bacteria particularly like to settle in the spaces between the teeth and spread from there to the gums. However, you can't get into the narrow spaces between your teeth with a normal toothbrush. That's why you should clean the spaces between your teeth once a day - ideally with an interdental brush.
Good to know:
Interdental brushes clean the often neglected interdental spaces. If you have gum problems in particular, you should clean daily with the right interdental brush to prevent infections and plaque build-up - for example with an interdental brush from Curaprox.
4. Use a tongue scraper
Bacteria can also settle and spread on the tongue. To do something good for your oral health, clean your tongue once a day with a tongue scraper. You can find out exactly how to do this and what the benefits are in our guide:
Using a tongue scraper correctly
5. Go to the dentist regularly
If you go to the dentist regularly for check-ups, your dentist can keep an eye on the health of your oral mucosa. Your dentist can identify things that could become problems, such as ill-fitting dentures or sharp tooth edges, at an early stage and intervene accordingly.
Ideally, you should also have your teeth professionally cleaned once or twice a year at . A dental professional will remove any tartar that is stuck in your teeth and in which bacteria are trapped. The dental hygienist also identifies dental damage. This means that if you have your teeth checked and cleaned regularly, you are investing in healthy teeth for the long term.
6. Pay attention to a healthy diet
Sugar is literally a favourite food for bacteria. If your diet is high in sugar, you are more likely to suffer from inflammation than if you prioritise a healthy diet and eat lots of fruit and vegetables. Switching to xylitol instead of sugar even helps your teeth and ensures a balanced blood sugar level.
There is also a direct link between aphthae and diet: people who regularly consume alcohol, sugar and processed foods or have a vitamin B12, iron or folic acid deficiency are more likely to suffer from nasty inflammations.
7. Increase the body's defences
In general, the stronger our immune system is, the better it can deal with unwanted intruders. To fight off bacteria, fungi and viruses and avoid oral mucositis in the future, you should therefore strengthen your immune system. You can do this by getting enough exercise - ideally in the fresh air, getting enough sleep and relaxing in everyday life. Visits to the sauna and alternating showers are also good for activating the immune system. And for the very brave: have you ever tried ice bathing or winter swimming?
8. Protect against infection
Not all oral mucosal inflammation is caused by bacteria or poor oral hygiene. If someone close to you suffers from aphthous stomatitis, caution is advised: After all, the viral infection is contagious. Do not share cutlery with the infected person, do not drink from the same bottle or glass and do not kiss the person.
9. Drink enough
If your oral mucosa is always well moistened with saliva, germs have less chance of settling and multiplying. This is because saliva has an important protective effect. However, if your mouth is dry because you don't drink enough or your saliva production has decreased due to illness, bacteria, fungi and viruses can take hold more easily.
Good to know:
Chewing gum stimulates saliva production and helps to combat dry mouth. The 'Black is white' chewing gum from Curaprox not only tastes deliciously fresh and limey, but also contains enamel-strengthening hydroxyapatite and activated charcoal for a gentle and natural whitening effect.
Sources
Altenburg, Andreas et al: Treatment of chronic recurrent oral aphthae, in: Deutsches Ärzteblatt. 2014.
Antwerpes, Frank et al: Aphthea and stomatitis at: flexikon.doccheck.com.
Gesund.bund.de: Aphthae.
Ferchland, Alice: Inflammation in the mouth: causes, symptoms and effective treatment methods, at: getmayd.com.
informedhealthonline.org: Fungal infection of the oral cavity (oral candidiasis).
Haas, Inga et al: Stomatitis aphthosa, at: flexikon.doccheck.com.
Hennessy, Bernard: Stomatitis, in: MSD Manual. Edition for healthcare professionals.
Paediatricians on the net: Mouth sores and oral thrush: Give children soft and cool food.
Dental medicine guideline: S2k guideline (long version): Diagnosis and treatment options for aphthae and aphthoid lesions of the oral and pharyngeal mucosa.
NDR: Preventing recurring aphthae through diet.
Austrian Public Health Portal: Stomatitis: Inflammation of the oral mucosa.
Remmerbrach, Torsten et al.: Diseases of the oral mucosa, on: zmk-aktuell.de.
All websites last accessed on 10/03/2024.
 Swiss premium oral care
Swiss premium oral care