Definition: What is oral thrush?
Oral thrush, or oral candidiasis, is caused by a group of yeasts (Candida), and the most common pathogen is a yeast fungus called Candida albicans. "Albicans" means "to whiten". The fungus is so named because it is characterised by a whitish coating.
Candida albicans colonises the healthy skin and mucous membrane flora of most people and is a common inhabitant in the normal microbiome of the oral flora, digestive system and vaginal area. The yeast fungus is usually not harmful to humans – at least not if our immune system is intact and can keep the fungus under control. However, if the immune system is compromised, Candida albicans can overgrow on mucous membranes or moist skin, particularly following chemotherapy, leukaemia or an HIV infection/AIDS. Antibiotics can also lead to the overgrowth of fungi in the intestines or vagina, resulting in fungal infections. If the pathogens multiply in the mouth, it is referred to as oral thrush or oral candidiasis.
Oral thrush is especially common in babies. Newborns are particularly at risk until they reach the age of about six-months-old. In children of this age, the colonisation of healthy germs on the mucous membranes is not yet balanced and thus creates favourable conditions for yeast fungi to thrive. In addition, the immune defences of babies are not yet fully developed, facilitating the growth of Candida albicans.
Where exactly does oral thrush occur?
The fungal infection can basically spread across the entire oral cavity and form an extensive white coating. Yet, this typically occurs only in the advanced stages of the disease. Individual areas are usually affected first.
These include:
- Tongue
- Palate
- Throat
- Gums
- Lips
- Corners of the mouth
A Candida infection can also manifest in the oesophagus. However, this is no longer referred to as oral thrush but as esophageal thrush.
What does oral thrush look like?
As briefly mentioned above, a whitish coating is characteristic of a fungal infection of the mouth. This coating may also appear grey. Parents frequently ponder whether the coating in their baby's mouth is oral thrush or simply "milk tongue". Since: A baby's tongue can also develop a temporary coating of milk residue, which is entirely normal and typically fleeting. Parents can easily distinguish between a fungal infection and milk residue, since oral thrush patches, unlike milk residue, cannot be wiped off without leaving behind red areas that may bleed slightly.
Good to know:
Patches or coatings on the tongue can have various causes. Read the following article to discover the possible reasons for a coated tongue. And here you can learn all about the phenomenon known as "geographic tongue".
Important tip: When checking for oral thrush in babies, perform this "test" gently, avoiding any excessive pressure on the coating. If it is oral thrush, trying to wipe it off may cause bleeding. Parents should also promptly consult a paediatrician if they notice any unclear or ambiguous signs. Oral thrush must be treated early to prevent it from spreading.
Suspected oral thrush: Which health care professional should I see?
Do you think you have oral thrush? If so, it is best to see your family doctor as soon as possible for early treatment. You can, of course, also consult an ENT specialist. Do you think your child is affected? In this case, a paediatrician should be your first point of contact.
Yeast infection of the mouth: How long does the healing process take?
It is obviously very important for those affected to understand the expected duration of their illness, especially considering the painful sensation often linked to oral thrush. Unfortunately, it is not possible to generalise about the course of the disease, but typically, sufferers might expect it to last roughly eight to ten days. Early detection and treatment of oral thrush are crucial nonetheless. When promptly addressed, the infection typically resolves without any complications in both children and adults.
A yeast infection can also be chronic. This condition is known as chronic mucocutaneous candidiasis, which is an hereditary immunodeficiency disorder. The cause lies in the malfunction of T cells (a type of white blood cell). As a result, the body struggles to defend itself against the yeast fungus Candida albicans. Antifungal medicines can usually control the chronic infection, but patients must take them over a long period of time.
Is oral thrush contagious? The transmission paths
Candida albicans, the yeast fungus causing infections, can be transmitted from person to person. As such, the disease is contagious. However, the infection is only transmitted if the skin or mucous membranes are damaged or the immune system is compromised. Unfortunately, it is not possible to provide information on the incubation period.
It can, for example, be passed from mother to baby during a normal birth. This is not uncommon. In the late stages of pregnancy, women are more susceptible to vaginal yeast infections. If the disease is actually present, the spores can potentially enter a child's mouth while being born.
The yeast fungus can also infect the nipples and might be transmitted to the baby through breastfeeding. A soother can also transfer yeast fungi if, for instance, an infected mother places it in her mouth before giving it to her baby.
Many people also wonder whether vaginal thrush (or a vaginal yeast infection) can be transmitted to the mouth. Yes, this is possible – for example during oral sex or if very poor hygiene standards exist.
With all these transmission paths, however, it must be emphasised that a yeast infection typically arises when existing pathogens, commonly present in our bodies, multiply unchecked on the oral mucosa, for instance because our immune system is not working properly and effectively.
How long is oral thrush contagious?
It is not possible to make a definite statement about this. Extra caution should be exercised as long as the white coating is still visible. Even afterwards, affected individuals should maintain stringent hygiene practices and avoid kissing others or sharing cutlery.
Oral thrush: Symptoms at a glance
Often, the disease initially manifests with a reddened mucous membrane. During this period, oral thrush might go unnoticed or be overlooked, especially in babies and small children. Over time, however, the disease becomes more noticeable. The lingual papillae (the tiny bumps that normally cover the surface of the tongue) may become less visible or even disappear completely in some cases. After a few days, whitish to greyish patches with a creamy consistency may emerge, which can be wiped off. A yellowish layer may also appear. As described briefly above: Wiping this coating off might result in the mucous membrane bleeding slightly. Individuals affected by this condition may also suffer from bad breath.
As the disease progresses, the lymph nodes may swell – indicating that the body has started to fight the pathogens. In addition, there is usually a painful feeling in the mouth. Babies might develop a fever and refuse to eat due to the discomfort caused by the damaged oral mucosa. Other symptoms associated with oral thrush can include a dry mouth, a burning sensation in the mouth and a loss of taste.
If oral thrush is not recognised and treated promptly, the pathogens might spread, leading to additional symptoms like nausea, vomiting and heartburn. The throat can also become inflamed if the fungus spreads along the oesophagus. Another symptom is hoarseness.
Causes: What causes the fungal infection of the mouth?
As mentioned earlier, the spread of the yeast fungus primarily occurs due to an impaired immune system. However, there are other causes and risk factors that can favour the onset of oral thrush:
- Being old
- Taking certain medications such as cytostatics, antibiotics, inhaled glucocorticoids (cortisone sprays), immunosuppressants
- Having dental caries
- Wearing dentures
- Having a dry mouth
- Eating a high-carbohydrate diet
- Smoking
In addition, stress can play an indirect role. Stress tends to weaken our immune system, making us more susceptible to illnesses. This can naturally facilitate the spread of pathogens like Candida albicans.
Good to know:
As the spread of yeast fungi can be favoured by dental decay, it is important to ensure optimal oral hygiene. Read the following article to find out how to brush your teeth correctly.
Treatment: How to combat oral thrush
What to do about a fungal infection of the mouth? Although the disease is usually harmless, it can be persistent and does not resolve on its own. If you or your child suffer from oral thrush, you will need medical treatment. In both children and adults, antifungal medicines, known as antifungals, are then often employed. Commonly used active ingredients for treating oral thrush include nystatin, miconazole or amphotericin B. Caution: Taking a course of these medicines may result in side effects like headaches or diarrhoea.
By the way, many of the medications for oral thrush are available over the counter at pharmacies without the need for a prescription. However, it is advisable to consult with a doctor before taking them.
The medicines, often available in the form of gels, ointments, lozenges, mouthwashes or suspensions, are applied directly to the white coating. It is, therefore, a localised therapy. Due to its ease of use, liquid nystatin is commonly prescribed for infants, who belong to the group most frequently affected by oral thrush. Parents can apply the medicine to the inside of the infant's cheek using a cotton bud or their finger.
However, if other organs such as the intestines are affected by the yeast fungus, localised treatment of the mouth is simply not enough. In these cases, a doctor will prescribe a more potent antifungal drug, such as fluconazole. This then exerts its effect throughout the entire body.
It is crucial that those affected take their medication over a sufficiently long period of time. Your doctor will inform you about the exact duration. Typically, treatment needs to be continued even after the white coating and other symptoms have subsided. This ensures that all the pathogens have really been destroyed.
Good to know:
If you seek medical attention for oral thrush, your doctor may use the ICD-10 code B37.0, which refers to Candida stomatitis. This code is part of the ICD classification system and may be found on your personal medical documents. This system is used to consistently label medical diagnoses in outpatient and inpatient care.
Home remedies and further tips for oral thrush
Can I treat oral thrush myself? No, an infection caused by yeast fungi usually requires treatment with prescribed medication, as previously stated. Nevertheless, there are home remedies and tips that can at least alleviate the painful, burning sensation and discomfort in your mouth. Especially for parents of babies, such tips can be invaluable in making the waiting time until you can see a doctor more bearable for their child.
Tincture of myrrh
Parents can dab a diluted tincture of myrrh on the affected areas in the mouth. However, it is important to wait at least one hour after taking or using the antifungal agent. Otherwise, irritations may occur. Adults can, of course, also apply this home remedy themselves.
Mouthwashes with arnica and sage
These two herbs are also believed to have a soothing effect on oral thrush. They are said to possess fungicidal properties and act as antiseptics, exhibiting anti-inflammatory effects. You can get them over the counter at a pharmacy. While natural remedies may provide some relief, it is crucial to note that they do not eliminate the disease entirely.
Avoiding sugar and yeast
Candida albicans loves sugar and yeast since the fungus feeds on them. During an acute illness, individuals should, therefore, abstain from eating sugar and yeast entirely to deprive the pathogen of its primary source of sustenance. Patients should also avoid fruit juices and acidic foods as they can be too aggressive for the oral mucosa and cause pain. Dairy products are not recommended either, as they produce mucus.
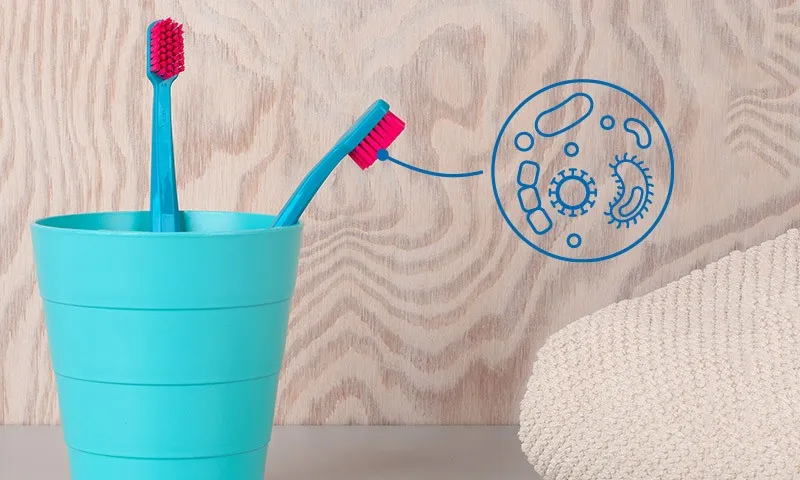
Taking oral hygiene very seriously
Yeast fungi not only love sugar and yeast but also our teeth, especially if they are affected by dental decay. They can feel right at home on unbrushed teeth, allowing them to thrive and propagate undisturbed. Oral hygiene is, therefore, the be-all and end-all when it comes to preventing oral thrush. It is recommended to also change your toothbrush more frequently than usual during an acute illness. Dentures or braces can be effectively cleaned using antimycotic (antifungal) solutions. Soothers should be disinfected and boiled on a regular basis.
Good to know:
Oral thrush can be very painful. Babies in particular are understandably reluctant to have their teeth brushed. However, as oral hygiene is a key factor in the fight against yeast fungi, finding gentle and positive ways to make teeth brushing more pleasant for children is crucial. The Curaprox baby toothbrush makes brushing their teeth especially pleasant. Its soft filaments ensure that your baby's mouth is not irritated.
Staying hydrated – but do not drink camomile
It is important to drink enough when suffering from oral thrush. Opting for water at room temperature is best. Camomile tea – a popular drink to combat many illnesses – should definitely be avoided when suffering from oral thrush. The tea is suspected of promoting the fungal infection of the mouth.
Do homoeopathic remedies help against oral thrush?
Homoeopathic remedies are very unlikely to effectively manage oral thrush for you or your child. There is, as yet, no scientific evidence to back up the effectiveness of globules and the like against the disease. Instead, place your trust in your doctor's advice and adhere strictly to the prescribed medication for oral thrush.
Preventative measures: Effectively preventing oral thrush
The most important preventative measure against the spread of Candida albicans is good oral hygiene. Both adults and children should clean their teeth regularly – at least twice a day. Moreover, it is imperative not to overlook the interdental spaces, where food debris, which yeast fungi love to feast on, may accumulate. Interdental brushes are best suited for cleaning the spaces between our teeth.
If you are prone to dental decay, you can also gargle with a mouthwash containing chlorhexadine from time to time. This has been proven to reduce germs and bacteria. And Perioplus+ Balance from Curaden not only provides an extra-strong protective film on your teeth but also ensures a fresh breath. But before getting started, you should always consult with your dentist first. Normally, a mouthwash is not necessary for daily dental hygiene; however, in certain situations, using chlorhexadine can be a sensible addition to your oral care routine.
Given that oral thrush often affects babies, breastfeeding mothers should prioritise regular cleaning and care of their nipples. By the way, there is no need to stop breastfeeding a baby with oral thrush. In this case, the mother only needs to pay more attention to keeping her nipples clean. Should the mother be afflicted with the fungal infection of the mouth, it is advisable to avoid direct contact with her baby's oral mucosa. And what should always be avoided becomes even more imperative: Never place a soother, bottle or spoon in your mouth before giving it to your child.
Sources
Gesundheitsinformation.de: Pilzinfektion der Mundhöhle (orale Candidose).
Kinder- und Jugendärzte im Netz: Mundsoor.
Leading Medicine Guide: Mundsoor: Informationen & Mundsoor-Ärzte.
MedLexi.de: Mundsoor.
MOOCI, Qualitätsgeprüfte Informationen & Ärtz:innen: Mundsoor.
Fernandez, James: Chronische mukokutane Candidose at: MSD Manual.
Universitätsspital Zürich: Candida albicans.
Pschyrembel online: Soorösophagitis.
All websites last accessed on 14 September 2023.
 Swiss premium oral care
Swiss premium oral care