Definition: What is hand, foot and mouth disease?
Hand, foot and mouth disease, or HFMD, is a highly contagious viral infection. Its symptoms usually include fever and a rash of blisters, which is commonly found on the hands and feet and in the mouth.
Only humans can catch hand, foot and mouth disease. Even though the name sounds very similar, the viral infection has absolutely nothing to do with foot and mouth disease that affects farm animals.
Frequency
Hand, foot and mouth disease is a global infectious disease that occurs throughout the year – meaning it can break out anywhere and at any time. The infection is common in children under the age of ten and is more prevalent in the late summer and autumn. As the disease does not have to be reported to local health authorities, no exact figures are available. The German National Association of Statutory Health Insurance Physicians estimates, however, that between 80,000 and 140,000 people in Germany catch the disease each year.
Symptoms & course
Hand, foot and mouth disease usually has the following course:
Incubation period
It usually takes three to ten days after infection before the first symptoms start to materialise. In an estimated 80 per cent of those infected – especially adults and children over the age of ten – the disease has a very mild course without any distress and discomfort. As such, many people do not even realise they are infected.
Good to know:
Even if they experience a very mild course without symptoms, infected individuals are still highly contagious. Therefore, if you think you have hand, foot and mouth disease, avoid close contact with young children as much as possible.
How does hand, foot and mouth disease start?
Even though the name clearly indicates which parts of the body will be affected during the course of the disease – hand, foot and mouth disease usually starts with unspecific, flu-like symptoms:
- Fever
- Nausea and vomiting
- Sore throat
- Aching limbs
- Lethargy
- Loss of appetite
- Feeling unwell
However, individuals with hand, foot and mouth disease might not get a fever at all.
Further course: Rash
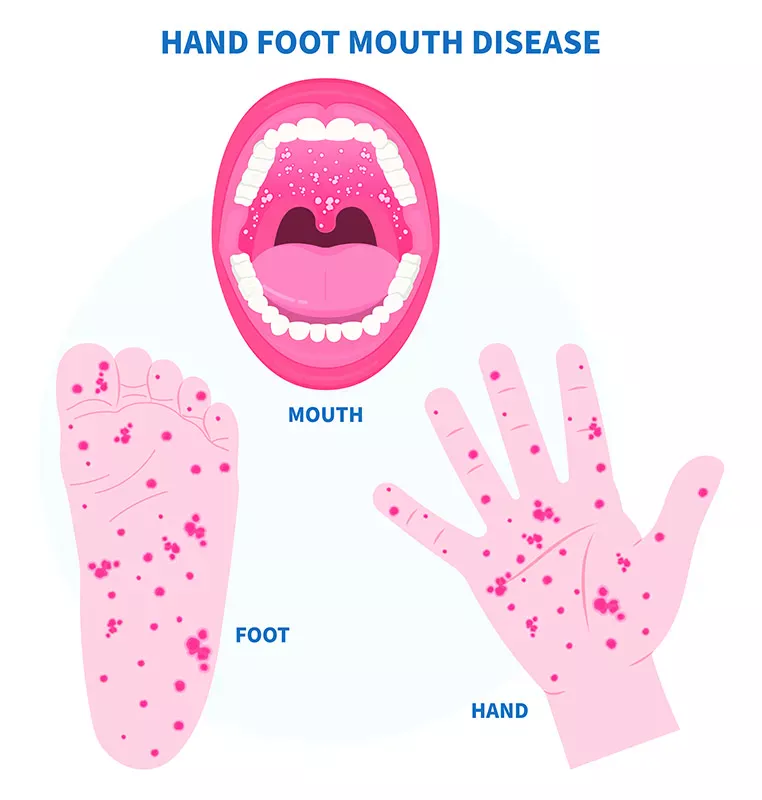
After one to two days, small red spots suddenly appear in the oral cavity – especially at the back, on gums and on the tongue – which later develop into whitish, fluid-filled blisters or aphthae. In young children, hand, foot and mouth disease is often indicated by the fact that swallowing is painful and they, therefore, "drool" more than usual to avoid swallowing. When the blisters inside the mouth burst open and release secretion, one of the side effects is bad breath.
A few hours or one to two days after developing a rash in and around the mouth, a rash of red spots appears on the palms of the hands and soles of the feet, sometimes with blisters. The blisters usually do not itch; although itchy blisters can also form. Moreover, the rash can also show up on the knees, elbows, buttocks and genitals. As the disease progresses, skin on the hands and feet starts to peel off.
Good to know:
Hand, foot and mouth disease can also occur without any blisters in the oral cavity. The blisters may then appear all over the buttocks. However, the shape of the blisters is the same on all parts of the body: They are generally white with a red border and filled with fluid.
Duration
Hand, foot and mouth disease usually gets better on its own seven days after the onset of symptoms.
Images
The following illustrations give a good indication of what hand, foot and mouth disease can look like.
Possible complications
In rare cases, fingernails and toenails may peel off about four weeks after the disease. But do not worry, new nails will grow back. Inflammation of the brain or meninges, paralysis and life-threatening lung, heart and liver issues are extremely rare. This normally only affects people that have a weak immune system.
What is the course of hand, foot and mouth disease among adults?
Coxsackievirus A6 hand, foot, and mouth disease can lead to usually more serious complications among adults. Besides a high temperature and flu-like symptoms, rashes may develop on the back of the hands and feet, lower legs and forearms. However, the typical blisters and oral aphthae do not occur with this variant.
When infected via other viruses – enteroviruses or another coxsackievirus A – the symptoms are normally less severe in adults. The disease course is often mild or even asymptomatic. However, in individuals with a weakened immune system, it can result in a severe illness.
If you are experiencing symptoms of hand, foot and mouth disease, always consult a doctor. They will decide how long you should stay at home to prevent it spreading to other people – especially young children. You can usually return to your normal routine after one week.
Is HFMD dangerous for babies?
If a mother becomes infected during pregnancy, the course of the disease is usually very mild or even asymptomatic, as in the majority of adults. This does not normally pose a risk to the unborn child. However, a mother may become infected shortly before giving birth, potentially transmitting it to the baby during delivery. As a rule, newborns do not suffer severe symptoms.
Very rare are severe courses of the illness: If the infection spreads, it can damage vital organs like the heart and liver and, in the worst case, lead to death. People are most at risk of contracting this systemic infection in the first two weeks of life.
There is no evidence that the viruses that cause hand, foot and mouth disease can be transmitted through breastfeeding, i.e. via breast milk. Consequently, there is no reason to stop breastfeeding your baby as a result of the disease. That said, infected mothers should practise good overall hygiene at all times and regularly wash their hands.
Causes: How is HFMD transmitted?
The causes of hand, foot and mouth disease have been well researched: The infectious disease is highly contagious, primarily spreading from person to person through enteroviruses, notably enterovirus A71 and coxsackievirus A. It is usually transmitted via droplet infection or smear infection. The fluid in the blister-like sores contains large amounts of the highly contagious viruses that cause HFMD, which can be transmitted through the air or by touching infected objects.
Droplet infection
In the case of droplet infection, the viruses enter the air directly via bodily fluids, such as saliva or nasal secretions, as tiny droplets – for example, when coughing or sneezing. Healthy individuals can become infected by inhaling these droplets.
Smear infection
If the blisters burst, the viruses they contain can also be easily transmitted to objects and surfaces, such as toys in nurseries, door knobs or cutlery, and lead to infection upon contact. This is the reason why hand, foot and mouth disease spreads very quickly, especially in nurseries when children share toys.
Contact with faeces
The viruses can also be transmitted through faeces. For instance, if an infected person fails to wash their hands thoroughly after going to the toilet, or if an adult comes into contact with faeces when changing an infected child's nappy. Smear infection with viruses from faeces is thus also possible.
How long does HFMD stay contagious?
The risk of infection is at its greatest when the fluid-filled blisters can burst. Children should therefore stay at home during the acute phase to minimise the risk of spreading the disease.
Once the rash has dried out fully, your child can go back to nursery or school. A certificate from a medical practitioner is not required, as hand, foot and mouth disease does not have to be reported to local health authorities. The viruses can still be transmitted through faeces for a number of weeks, but the disease is unlikely to be passed on in this manner.
Is it possible to be reinfected?
Once you have had hand, foot and mouth disease, you or your child will develop immunity to the pathogen. That said, you can still become reinfected, since there are roughly 15 different viruses that can cause the disease.
Good to know:
It is probably best not to travel with your child during the acute phase to avoid spreading the infection to others at your holiday destination. Otherwise, there is a good chance of hand, foot and mouth disease breaking out in the hotel you are staying in. Should your child contract the disease on holiday, doctors recommend avoiding sun exposure during the acute phase and being rigorous about sun protection once the symptoms have abated.
Diagnosis: When should you consult a health care professional?
If you are worried about your or your child's symptoms of hand, foot and mouth disease, it is advisable to consult a paediatrician or your family doctor to rule out any other diseases that present similar symptoms. There are a number of illnesses that can lead to blisters forming in your mouth. They include, for example, herpes, tonsillitis and glandular fever.
Usually, a doctor can make a confident diagnosis by examining the rash and asking whether your child has been in contact with anyone infected. Further examinations are not usually required. In severe cases or when symptoms are nonspecific, the health care professional may take a blood or stool sample or swab the blisters or throat. In very rare cases, a doctor might also take a sample of the cerebrospinal fluid.
Normally, hand, foot and mouth disease is best treated at home. Only in the most extreme of circumstances does HFMD require hospitalisation.
Treatment: What helps against HFMD?
At present, there are no medicines to cure hand, foot and mouth disease. Which is nothing to worry about, as the disease usually gets better on its own in roughly seven days. However, to speed up the healing process, you can take over-the-counter drugs or use home remedies. We have put together an overview for you below:
Medications
To relieve symptoms, you can take antipyretics and painkillers, such as paracetamol – best given to babies and toddlers as suppositories. Pain-relieving mouthwashes and gels containing chlorhexidine or lidocaine or even a Bepanthen solution can help with the oral blisters and alleviate discomfort with swallowing. Have a word with your paediatrician or family doctor to discuss the best medications for treating hand, foot and mouth disease and to get a prescription. Antihistamine medicines can be taken to reduce severe itching of the hands and feet. However, this is rarely required, as the blisters do not cause itching as a rule.
Antibiotics are ineffective, as they are used to fight bacterial infections only. Sometimes, however, people can develop a bacterial infection in addition to the viral one. In this case, antibiotics would be a good idea.
Good to know:
Acetylsalicylic acid (ASA, the active ingredient in aspirin), a very popular analgesic and antipyretic drug, should not be given to children with hand, foot and mouth disease. In combination with the viral infection, severe complications can arise.
Home remedies: Eight tips for treating hand, foot and mouth disease
Use these tips to relieve acute symptoms while your child is sick and to speed up the healing process:
- Besides antipyretics, you can use wet leg compresses to suppress fever during the infection.
- Make sure your child drinks enough – despite the illness making it painful to swallow. Otherwise there is a real risk of dehydration.
- If your child is reluctant to eat, try pureed foods, custard, yoghurt or soups, as these soft options are much easier to swallow.
- Anti-inflammatory zinc-oxide lotions and other ointments and gels containing zinc can help dry out the blisters.
- Cold chamomile or marigold tea or plant-based lotions (for example, lemon balm, thyme or chamomile) can alleviate oral discomfort.
- Gently dab a honey-soaked cotton swab on the painful blisters in your mouth. This also helps relieve the pain caused by the sores.
- Ice lollies have a pleasant cooling effect and help prevent dehydration of the oral mucosa.
- With blisters in the mouth, it is probably best to avoid acidic drinks, such as fruit juice. The acid further irritates the oral mucosa and simply makes the pain worse.
Good to know:
Despite experiencing painful sores in their mouth, it is essential for your child to maintain proper oral hygiene. Clean their teeth carefully with a soft toothbrush and a mild toothpaste. The Curaprox baby toothbrush and the Curaprox children's toothbrush feature more than 4,260 and 5,500 super soft filaments respectively, thereby ensuring gentle yet thorough cleaning. Further, the Curaprox kids toothpastes are extremely mild and do not contain any harmful substances.
Natural remedies
Some people swear by homoeopathic or spagyric remedies and prefer to treat hand, foot and mouth disease with globules or spagyric sprays. For example, the homoeopathic remedy Rhus toxicodendron is said to combat the blisters, while Apis and Belladonna are generally used to relieve fever. In this case, it is best to seek advice from an alternative health practitioner. However, please keep in mind that there is no scientific evidence to back up the effectiveness of homoeopathic or spagyric treatments and any improvement is most likely down to a 'placebo effect'.
Preventative measures: How can you avoid catching hand, foot and mouth disease?
Seeing as there is no vaccine against hand, foot and mouth disease, good hygiene is the key to protecting yourself against an infection:
- Remember to wash your hands after going to the toilet or changing your baby's nappy, but also before and after preparing food and after blowing your nose, coughing or sneezing – always wash with soap and water for at least 30 seconds.
- Avoid close contact with people who are infected – do not hug or kiss them.
- Clean and disinfect frequently touched surfaces and objects, such as toys, door knobs and taps.
- Do not share glasses, cups and cutlery.
Sources
Antwerpes, Frank et al.: Hand-Fuß-Mund-Krankheit, at: flexikon.doccheck.com.
Böhm, Ariane: Hand-Mund-Fuß-Krankheit bei Erwachsenen – erkennen, at: rbb-online.de.
Centers for Disease Control and Prevention: Hand, Foot, and Mouth Disease (HFMD).
Gesundheitsinformation.de: Hand-Fuß-Mund-Krankheit.
Herzner, Simone: Hand-Fuß-Mund-Krankheit: Was hilft?, at: apotheken-umschau.de.
Infektionsschutz.de: Hand-Fuss-Mund-Krankheit.
Liu, Zhihui et al.: Association of Short-Term Exposure to Meteorological Factors and Risk of Hand, Foot, and Mouth Disease: A Systematic Review and Meta-Analysis, in: International Journal of Environmental Research and Public Health. 2020.
Löwen-Apotheke: Hand-Fuß-Mund-Krankheit.
Mutter + Kind Ratgeber: Hand-Fuss-Mund-Krankheit.
Robert Koch Institut: Hand-Fuß-Mund-Krankheit (HFMK).
Sinowatz, Fabian: Hand-Fuß-Mund-Krankheit, at: netdoktor.de.
Universitäts-Kinderspital Zürich: Hand-Fuss-Mund-Krankheit. Notfall-Elterninformation.
World Health Organization: A Guide to Clinical Management and Public Health Response for Hand, Foot and Mouth Disease (HFMD).
All websites last accessed on 7 July 2023.
 Swiss premium oral care
Swiss premium oral care