The most important facts in brief
- Peri-implantitis is when the area around an implant has become inflamed and the pathogenic bacteria have already penetrated into the deeper tissues.
- Peri-implantitis often develops unnoticed from an inflammation of the oral mucosa.
- Symptoms are often not felt at first. Later, the affected area is often sensitive to pressure. Pus may also form at this point. As the condition progresses, those affected suffer from increasing pain.
- The best protection against the bacterial-inflammatory disease is exemplary oral hygiene.
- If peri-implantitis is recognised at an early stage, it may be sufficient to have one or more professional dental cleanings carried out and to clean and care for the implant and the rest of the oral cavity particularly intensively.
- Advanced infections can lead to bone resorption and, in the worst case, to the loss of the implant. More complex therapies are then necessary.
Definition : What is peri-implantitis?
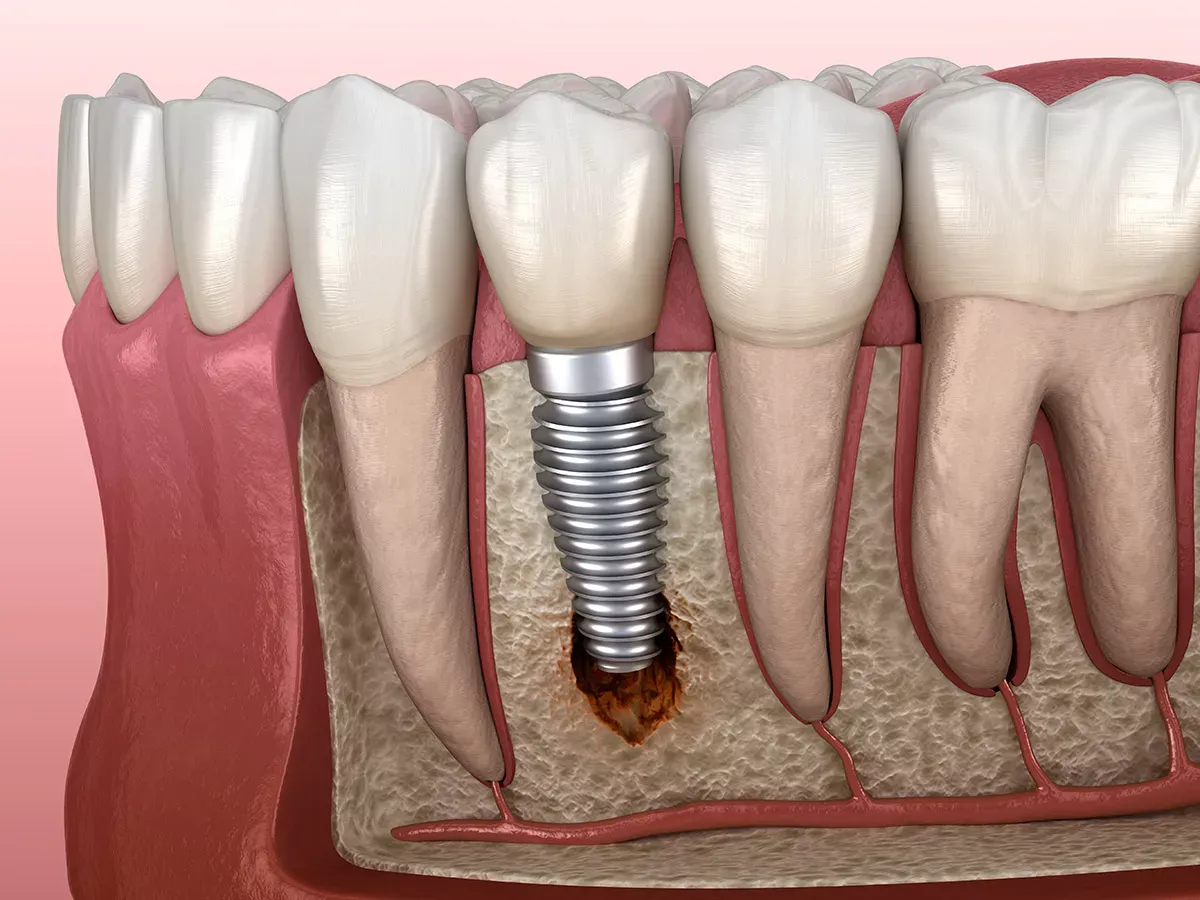
People suffer from peri-implantitis when the area around a dental implant becomes inflamed. The prefix "peri" comes from the Greek and stands for "around/about". The "itis" describes the inflammation.
Frequency of peri-implantitis
Regarding prevalence, i.e. the question of how many people are affected by peri-implantitis, it can be said that the figures vary greatly. According to the S3-guideline on the treatment of peri-implant infections on dental implants, it occurs on average in around 22 per cent of all implant recipients in Germany.
How does peri-implantitis develop?
Peri-implantitis is caused by bacterial plaque that has accumulated around an implant anchored in the bone, for example. This plaque is simply plaque that has not been removed by brushing.
The plaque bacteria can now cause some damage in our mouth: It often starts with a superficial inflammation of the mucous membrane around the dental implant - also known as oral mucositis. At this stage, many of those affected feel no or only very few symptoms (e.g. minor sores in the mouth) and therefore see no need for treatment.
However, if the bacteria now work their way deeper unnoticed, they also infect the tissue around the implant screw - and then, in the worst case, the jawbone. If the inflammation remains untreated, the tissue and bone will eventually break down. This is because our body recognises the inflammation and the immune system is now working at full speed. It not only attacks the plaque bacteria, but also its own tissue in the area surrounding the inflamed area.
If the bone then degrades, the anchoring of the implant is no longer present, causing the dental implant to loosen. In the worst case scenario, the implant may be lost.
As you can already see from the course of the disease: Early treatment can prevent the worst from happening. If peri-implantitis is recognised in its early stages, it can be easily cured.
Good to know:
Very good oral hygiene is the be-all and end-all when it comes to preventing peri-implantitis. But how do you take optimum care of your mouth and teeth? Here you will find comprehensive instructions on how to brush your teeth properly.
Peri-implantitis: causes and risk factors
As you have already learnt, plaque bacteria cause inflammation in our mouths, which can later spread to deeper tissues. The most common cause is therefore a lack of oral hygiene, which makes it particularly easy for plaque bacteria to spread in the mouth. However, there are also other reasons that can cause or favour the development of peri-implantitis.
Smoking
Smokers have an increased risk of developing inflammation on their implants. Why? Their blood vessels constrict as a result of cigarette consumption, which worsens blood circulation - including to the gums. This makes it easier for plaque bacteria to spread and cause inflammation such as peri-implantitis.
General diseases
Some diseases such as diabetes and osteoporosis can favour the development of peri-implantitis. In the case of diabetes, this can be the case if the patient's medication is not optimally adjusted. In the case of osteoporosis, the use of bisphosphonates (active ingredient that inhibits bone resorption) is a risk factor because they can reduce the local immune defence and bone regeneration.
Persistent stress
If we are constantly under stress, this has a negative effect on our entire body. Our immune defence drops and we are generally more susceptible to illness - including the development of inflammations such as peri-implantitis.
Irregular dental check-ups
Patients who have received an implant should take regular check-ups and aftercare appointments seriously. This is especially true for the first few months after the implant has been inserted. In this way, the dentist can monitor the so-called healing of the implant and recognise possible early signs of peri-implantitis.
In addition, your dentist will probably recommend an annual x-ray check-up, during which he can visualise inflammatory processes that are invisible from the outside.
There are also certain saliva tests that can be used for early detection. Ask your dentist for advice on the extent to which such a test is necessary for you.
Good to know:
Would you like to know how useful an X-ray examination at the dentist is and how harmful X-rays can be for you? Then read our article:
Symptoms of peri-implantitis
Different symptoms occur depending on the stage of peri-implantitis. As already described, in the initial phase there is often a superficial inflammation of the oral mucosa, which frequently causes no or only very mild symptoms. Sometimes the gums around the implant or the gums are swollen - the first noticeable signs of inflammation.
From this initial inflammation of the oral mucosa, the plaque bacteria responsible for the inflammation can now work their way quite quickly and fluently into the depths around the dental implant. If this is the case, peri-implantitis has developed. Patients are then likely to suffer from one or more of the following symptoms:
- Bad breath
- Pus formation at the inflamed site
- Pain when brushing your teeth
- Bleeding gums
- Gum recession ( Periodontitis )
- Bone recession and the resulting visibility of the upper part of the implant (only visible in the X-ray image)
- Implant loosening or loss
How peri-implantitis is diagnosed
If you notice one or more of the above symptoms, you should make an appointment with your dentist and not try to diagnose yourself. Of course, there are plenty of pictures on the internet, of what peri-implantitis can look like. However, you shouldn't let this impress you too much. Your dentist is the only person who can make the diagnosis and recommend the right treatment if necessary.
The dentist needs a so-called periodontal probe for diagnostics. It looks like a thin metal tip with which the dentist can measure the pocket depth. The pocket depth is the natural groove between the tooth and gum, which is up to 3.5 millimetres deep in a healthy state. The pocket depth can be measured with the periodontal probe. If it is too deep, this is an indication of peri-implantitis, as such deep pockets indicate bone loss.
The assumption can be confirmed with an X-ray. This is the only way to determine the extent of bone loss around an implant.
Your dentist may also want to carry out a laboratory test to determine which bacterium of the many hundreds of species in your mouth has caused the inflammation around your implant. With the help of such a bacteriological examination, the doctor can prescribe the appropriate antibiotic if such treatment is actually necessary for you - for example the local antibiotic Ligosan.
Diagnosis of peri-implantitis in ICD coding
If you go to the doctor as a patient with health insurance and they diagnose you with peri-implantitis, you will find the diagnosis in the doctor's letter as a so-called ICD -10-GM coding. ICD stands for "International Statistical Classification of Diseases and Related Health Problems". In German: International Classification of Diseases. Peri-implantitis is coded with the ICD code K05.1 / T85.78 ("Infection and inflammatory reaction caused by other internal prostheses, implants or transplants").
Treatment options: Stopping and treating peri-implantitis
Have you been diagnosed with peri-implantitis? Then your dentist will recommend a suitable treatment for you to prevent serious consequences such as bone loss and the loss of the implant. Which treatment makes sense in your case depends primarily on how quickly you visited the dentist, i.e. how far the peri-implantitis has already progressed.
Treatment in the early stages
Professional teeth cleaning
In the early stages, when only the gums are inflamed, it can already help if the cause - i.e. the plaque bacteria - is removed by a professional dental cleaning. With a bit of luck, the affected area will recover and you won't need any further treatment. However, your dentist may recommend shorter intervals between professional dental cleanings to prevent re-inflammation or to recognise it early enough.
Intensify oral hygiene and minimise risk factors
He will also advise you to reconsider your oral hygiene and invest even more time in it. After all, it has been proven that those who take good care of their teeth and gums and clean them regularly are less likely to develop peri-implantitis. Of course, you should also take care to minimise your individual risk factors for the development of inflammation. Smokers, for example, should avoid cigarettes altogether.
Mouth rinses for support - after consultation with a doctor
Are you wondering whether you should use a rinsing solution or ointment to help the inflammation around an implant heal more quickly? With the right choice, you can actually support the healing process. Choose rinses with chlorhexidine, but be sure to discuss the application with your dentist beforehand. This also applies to the use of mouth rinses with hydrogen peroxide. They are often used to clean wounds and for bleeding gums and inflammation of the oral mucosa. Before using them, be sure to ask how useful they are in your individual case.
Good to know:
For peri-implantitis symptoms in the mouth such as inflammation with pus formation on the implants, it can be helpful to use a disinfectant gel with the active ingredient chlorhexidine - for example, Perio Plus Focus Gel from Curaprox. A special anti-bacterial toothpaste such as Perio Plus Support toothpaste can also be used temporarily to keep the infection at bay and support the healing process. As always, however, you should first discuss with your doctor whether it is appropriate for your individual case.
It is important to know that mouthwashes should not be part of your standard oral hygiene routine. If your mouth is completely healthy, it does not require any additional rinsing in addition to normal tooth brushing. However, in the presence of diseases such as peri-implantitis, the use of mouthwashes for a certain duration can be beneficial.
Laser treatment
Laser treatment can also help to combat peri-implantitis. With lasering, germs that are responsible for the development of the inflammation can be killed. Ask your doctor for advice on whether and which laser therapy is suitable for you.
Treatment in more advanced stages
If advanced peri-implantitis has already attacked the jawbone and perhaps already loosened the implant as a result, the treatment is more complex. If a great deal of bone substance has already been lost, bone augmentation (regenerative therapy) is usually required. This is an oral surgery operation in which bone replacement material is inserted into the maxillary sinus. The aim is to use the rebuilt bone to create a new anchor for the implant and save the implant in this way.
This replacement material can be taken from neighbouring jaw regions such as the upper and lower jaw ridge or chin. Today, however, doctors often use other materials to spare patients the need to remove bone. Today, there are already many materials that come very close to human bone. For example, animal bones, coral or algae are added to them. If bone augmentation is successful, an implant can usually be inserted again.
Important to know: Both in the initial stage and in advanced phases, it is always essential to clean the teeth, the entire oral cavity and, of course, the implant. The tissue can only recover if the pathogenic plaque bacteria are removed. Some dental practices use the electrolytic cleaning procedure GalvoSurge to clean implants. The principle behind this is a low-level electrical voltage applied to the implant and spraying the implant with a cleaning fluid. This leads to the splitting of water into H+ and OH ions. This produces atomic hydrogen, which aggregates to form bubbles. These bubbles lift the pathogenic biofilm from the implant surface.
Whether your dentist uses the GalvoSurge method and to what extent it makes sense in your case is best discussed with them personally.
Healing time for peri-implantitis
Are you wondering how long you will have to deal with peri-implantitis? Unfortunately, it is not possible to give a general prognosis for the healing time. It depends on the stage of the disease. If the inflammation is detected and treated early, there is a good chance that you will soon feel better. However, if it is at an advanced stage, more extensive measures such as bone augmentation will often be necessary, so you will probably need longer to recover from the inflammation and its consequences.
Costs of peri-implantitis treatment
If you suffer from peri-implantitis, your health insurance company in Germany will cover some of the treatment costs. This means, for example, the costs for the X-ray, the examination or any antibiotics you may need to take.
Bone augmentation, which is necessary if your peri-implantitis is already very advanced, is not usually covered by health insurance. You will have to pay for this treatment yourself, just like the implant - unless you have supplementary dental insurance that subsidises this treatment.
To avoid any nasty financial surprises, you will receive a cost estimate from your dentist before treatment begins. In this statement you can see exactly how much money you will have to pay for what.
Home remedy : Treat peri-implantitis yourself?
Has an inflammation formed around your dental implant? Then you should make an appointment with your dentist immediately. Peri-implantitis is not to be trifled with. However, to bridge the waiting time until your appointment, you can try to get any pain under control with home remedies or simply regain a little sense of well-being. We have summarised the possible options for you:
Chamomile tea
Chamomile tea has an anti-inflammatory and antibacterial effect. If you gargle with cooled tea or simply rinse your mouth with it, you may be able to alleviate your symptoms. Alternatively, you can soak cotton wool in the tea and dab it on the inflamed area.
Carnations
In the case of peri-implantitis, the area around your implant is inflamed. This means that the inflammation is usually very localised. This does have the advantage that you can try cloves as a home remedy. To do this, carefully bite the clove on the painful area. This releases so-called eugenol. This substance has an analgesic effect.
Salt
Salt has disinfectant properties and can dissolve some of the tension in soft tissue. To benefit from this, you can dissolve some salt in a glass of warm water. Make sure you let the water cool down and rinse your mouth with it for a maximum of two minutes. Please spit the water out again. You can repeat this procedure several times.
Homeopathy? No proven effect
Alternative healing methods such as homeopathy are popular, but ineffective. At the very least, there is no evidence to date that you can defeat inflammation with them. Of course, you can take globules and the like and you may even feel a placebo effect, but there is no way you can avoid medical treatment. If you have peri-implantitis, it's best to go straight to the dentist.
Prophylaxis: how to take the right precautions
Peri-implantitis is primarily caused by bacteria, which we can remove quite reliably with good dental hygiene. The most important part of prevention is therefore exemplary oral hygiene. This includes brushing your teeth twice a day and not forgetting the spaces between your teeth. The quickest and most effective way to clean them is with interdental brushes.
Good to know:
After implantation, the interdental spaces are often larger than before. Curaprox has developed the Refill Implant interdental brush especially for implant wearers. With their fine and long bristles, the brushes are suitable for any size of interdental space.
Implant wearers should also take their dental check-ups very seriously. Peri-implantitis has the trick of being symptom-free at first, so it is important to have your mouth checked regularly by a dental professional in order to make an early diagnosis.
To avoid inflammation around your implant, it also helps to take a critical look at your lifestyle. If you smoke, you should stop or cut down as far as possible. Cigarette consumption is one of the risk factors in the development of peri-implantitis.
Sources
Compledent Dental Clinic: Peri-implantitis.
Deutsche Apotheker Zeitung: Successful treatment of peri-implantitis - is it possible?
Dr Kraus Implant Clinic: Peri-implantitis.
Fretwurst, Tobias et al: New findings on peri-implantitis at: www.zmk-aktuell.de.
Society for Dental Health, Function and Aesthetics: Peri-implantitis: A problem of the present and future and: Peri-implantitis: Inflammation at the dental implant.
Gesund.bund.de: What are ICD and OPS codes?
Heugel, Philipp - Oral and maxillofacial surgery: Peri-implantitis - inflammation around a dental implant.
Implants.com: Causes and risks of peri-implantitis and mucositis.
Leading Medicine Guide: Peri-implantitis: Specialists and information.
Matthias Teel Dental practice: Preventing peri-implantitis.
Mooci: Peri-implantitis.
Onko Internetportal: Oral mucositis as a side effect of cancer therapy.
Quintessence Publishing Germany: Clean implants thoroughly and gently with GalvoSurge.
Rößler, Ralf: Consistent diagnostics - avoidance of peri-implantitis and: Peri-implantitis: Local antibiotics to support therapy at: www.zwp-online.info.
All websites last accessed on 30.10.2023.
 Swiss premium oral care
Swiss premium oral care