Definition of caries: What is it actually?
Caries is a disease of the tooth caused by bacteria. The term "caries" is derived from Latin and means "rottenness or decay".
One characteristic of caries, and also its most noticeable indicator, is the much-feared cavity (hole) in the tooth, which becomes apparent only in the later stages of development. Unfortunately, caries is not uncommon: it ranks among the most common human diseases, alongside colds and gum disease. And what many people do not know: caries can be contagious. For instance, if parents with caries lick a spoon before giving it to their baby, there is a risk of the cavity-causing bacteria being transmitted from the parents' mouth to the child's mouth.
What causes caries to develop?
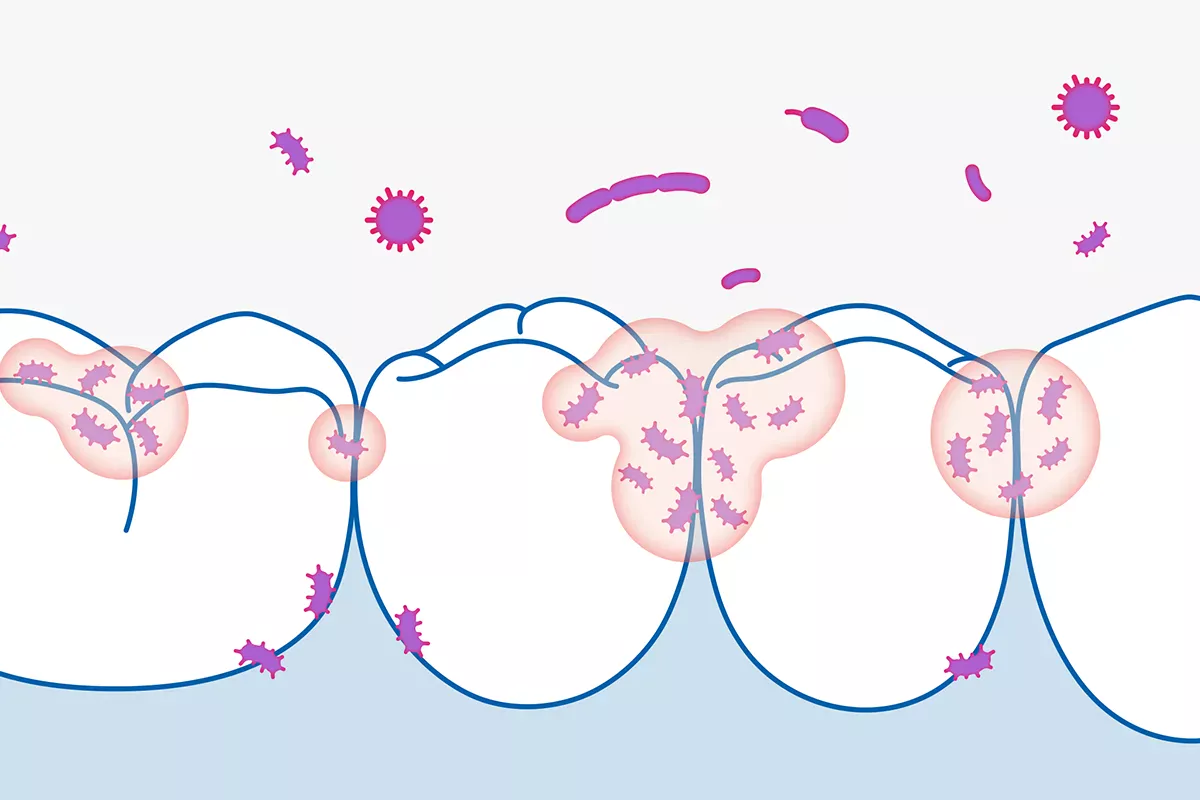
Be it a canine tooth, a wisdom tooth or even a milk tooth, caries can develop on all of our teeth, typically when we fail to brush them thoroughly and regularly. If this is the case, a coarse, furry-like coating known as plaque accumulates on the teeth. This predominantly white-yellowish coating is composed of saliva, bacteria and food debris. Initially, plaque is quite soft, making it easy to remove with a toothbrush and interdental brushes. Failure to do so, however, results in it turning into hard tartar, necessitating professional removal at a dental practice.
Bacteria within the plaque are the main culprits causing caries. These bacteria derive their energy from the carbohydrates found in our food. And they have a preference for readily fermentable sugars, which they convert into acids that erode the tooth enamel through demineralisation. This makes the enamel porous and thus more vulnerable to microorganisms that can infiltrate the tooth and lead to decay.
The good news: actually, there is an ongoing process in our mouths that safeguards our teeth against caries. Since our saliva is naturally enriched with minerals, which continually harden (remineralise) the tooth enamel. However, this natural process is sadly disrupted when we regularly consume sugar, whether in the form of frequent snacks or sugary beverages. In such cases, we subject our teeth to a constant onslaught of sugar, preventing saliva from adequately restoring the correct balance. This disrupts the remineralisation process and eventually leads to the formation of cavities.
To prevent this from happening in the first place, there is, as mentioned above, one simple yet important rule: brushing your teeth in the morning after breakfast and at night before going to bed, along with the use of a tongue scraper and suitable interdental brushes, helps eliminate the oral bacteria responsible for caries.
Good to know:
Caries is mainly caused by insufficient dental hygiene. But: some individuals have an increased susceptibility to developing cavities than others. This is due to the varying levels of acidity (pH) in our saliva. When this value is very low, it opens the gates and welcomes caries in.
Types at a glance: Where does caries occur?
Caries is referred to by various names, depending on where it occurs. Read about the distinctions made by dentists here.
Approximal caries
This term refers to caries that forms between teeth, specifically on the contact surfaces of two adjacent teeth. These spots are particularly vulnerable, as they are often overlooked during the cleaning process. However, they can be cleaned very effectively with interdental brushes.
Pit and fissure caries
This term refers to caries that develops on the tooth, specifically on the chewing surfaces of the molars. Typically, the root cause of this caries is inadequate hygiene or an incorrect brushing technique.
Smooth surface caries
This term refers to caries that develops on the side of the tooth, specifically on the surfaces facing the tongue, palate and buccal mucosa.
Cervical caries
This term refers to caries that develops on the exposed necks of teeth. Cervical caries is more common among older individuals, especially those with receding gums and exposed necks. The neck of the tooth is then no longer protected and becomes vulnerable to the disease.
Secondary caries
This term refers to caries that develops in areas that have previously undergone treatment. Thus, the new caries forms in the vicinity of dental fillings and crowns, also underneath a dental filling or crown. This is also referred to as recurrent caries. It is usually caused by poor primary care. Meaning that not all the caries-affected areas were completely removed during initial treatment.
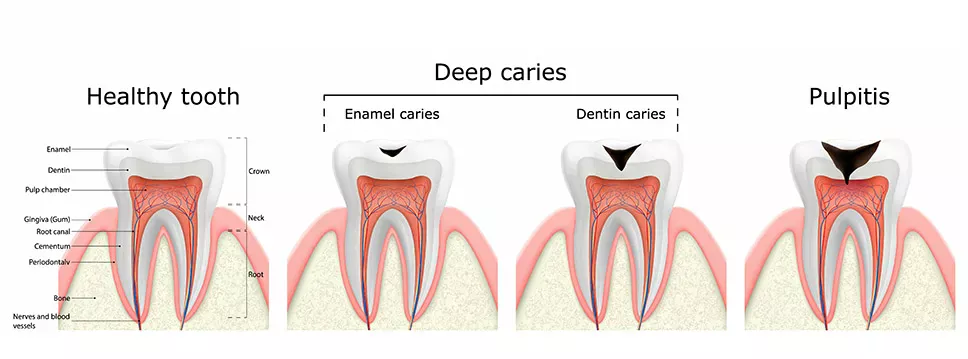
The various stages of caries
A cavity, or hole, never appears overnight. Caries development is more of a process that, ideally, can be detected and stopped early on. Find out about how caries develops and the various stages into which its course can be divided below.
Initial caries
Actually, initial caries represents only a preliminary stage of the disease, which may progress into full-blown caries without proper treatment. Initial caries typically manifests as white, brownish or translucent spots on teeth. These spots occur when the tooth enamel has already been attacked and the affected areas demineralised. The good news: At this stage of the disease, the damage can still be reversed.
Superficial caries
At this stage, the tooth has already suffered further damage; nonetheless, the tooth enamel has still "only" been affected by a superficial attack up to now. This damage now creates an ideal "nest" for bacteria to reside in, accelerating the progression of the disease.
Dentine caries
Dentine is the term used to describe the tissue located beneath the tooth enamel. This tissue is soft and, therefore, more susceptible to caries. When caries has already reached this part of the tooth, individuals often experience it as tooth sensitivity, especially when eating and drinking hot and cold items.
Deep caries (caries profunda)
In this case, the caries has already attacked two thirds of the dentine and extended into the pulp. The blood vessels and nerves are located in this innermost layer. Caries in this region can lead to irritation and inflammation of the pulp, resulting in significant pain. Root canal treatment is then often unavoidable.
Extremely deep caries (caries penetrans)
This is the most severe form of caries; virtually the final stage. The destructive bacteria have reached the pulp and created a connection between the oral cavity and the tooth cavity. If caries is not treated at this stage, there is a risk of pulpitis – inflammation of the pulp – and subsequent necrosis of the pulp.
Abscess
If caries has already reached the pulp, an infection can develop, potentially leading to the formation of an abscess beneath the tooth. An abscess of this nature is very dangerous and must be treated immediately. If left untreated, the infection can spread to the jaw bones and also to the head and neck. This often causes body aches and pain. Swelling of the gums, face or jaw may also occur. Fever and swollen lymph nodes can also indicate an abscess. In some cases, the impacted tooth may need to be extracted.
Risk factors and causes of caries
You have already learned about the most critical risk factors of caries: Plaque and tartar. However, there are also other factors that can contribute to the development of caries. We have put together a comprehensive overview for you below:
Insufficient dental hygiene
One thing in particular really helps in combating the bacteria responsible for caries: Getting rid of them. Make sure to brush your teeth for at least three minutes twice a day. And do not forget the spaces between your teeth. They are best cleaned daily using interdental brushes.
Good to know:
To prevent caries attacking the interdental spaces, it is crucial to clean them regularly. Using interdental brushes from Curaden, you can easily reach even the smallest nooks and crannies. You will find the right size for all your interdental spaces.
Too many sweet things
Most people have a sweet tooth. Unfortunately, this comes with the drawback of attracting "bad" oral bacteria, which derive their energy from these food sources, consequently causing caries.
Not enough fluoride in the tooth
As we are already aware, bacteria render our enamel porous and permeable, ultimately leading to the internal destruction of the tooth. Fluorides can help counteract this process. These are what are known as fluorine compounds. They are only found in very small quantities in food (exceptions are, for example, green and black tea and seafood), and water also only contains very few traces of fluoride. Meaning, we have to "replenish" them. This can be achieved, for instance, using toothpastes enriched with fluorides. In addition, various salt varieties with fluoride additives are available on the market – and this also applies to some types of mineral water.
Good to know:
In regions with higher fluoride levels in drinking water, the rate of caries is indeed lower than in other regions. If you are interested in delving deeper into the effects of fluoride, feel free to continue reading here:
Reduced flow of saliva
As we already know: Our saliva helps protect our teeth from caries. So, a reduced flow of saliva obviously increases the risk of cavities. For instance, specific medications can lead to decreased saliva production, as can radiation therapy as part of cancer treatment. Systemic diseases that cause salivary gland dysfunction can likewise result in reduced saliva production.
Genetic defects in the tooth enamel
Only intact, hard tooth enamel is a successful barrier against cavity-causing bacteria. Studies have revealed that mutated genes can be a contributing factor to weakened or defective tooth enamel. Individuals prone to caries should be particularly vigilant about maintaining excellent oral hygiene and place greater emphasis on regular professional check-ups.
Good to know:
During pregnancy, pregnant women are particularly susceptible to caries and even gum disease. This is often caused by hormonal changes. For example, you may have heard: "That you lose a tooth for every pregnancy." To prevent this from happening, pregnant women should be especially mindful of their dental hygiene. You can find out more here:
Do I have caries? Symptoms at a glance
The majority of people typically associate caries with pain and a visible cavity, or hole, in the tooth. Although both of these symptoms are indicative of an already advanced stage of caries. Caries in its initial stages is often not that easy to detect, underscoring the significance of regular dental check-ups. We have summarised the symptoms that can serve as indicators of caries for you below.
Sensitivity to hot and cold
An early sign of caries might be that you suddenly experience discomfort when eating or drinking hot or very cold items. If this is the case, you should go and see a dentist. Only a dentist can determine whether caries is the underlying cause. Since such sensitivity can also stem from other conditions, such as the exposed necks of teeth or periodontitis (inflammation of the periodontium).
Pain when eating sweet foods
Individuals with caries may experience sensitivity when their teeth come into contact with sweet foods. This is because the disease damages the enamel at a particular spot, creating a pathway to the nerve. Sugars irritate the nerve and cause pain and discomfort.
Toothache
Whether toothache develops or not can also be influenced by the exact location of the cavity. Cavities in the tooth enamel, for instance, usually do not induce pain. Spontaneous toothache, which occurs without any apparent cause like cold, heat or sweet items, typically only flares up when the cavities have reached or almost reached the pulp, or when the pulp is already affected. In most cases, this means that irreversible damage has been done.
Bad breath
Advanced caries can also cause bad breath. This is usually due to cavity-causing bacteria that have not been adequately removed. Food debris accumulates in existing cavities, which are metabolised by the bacteria, giving rise to malodorous sulphur compounds.
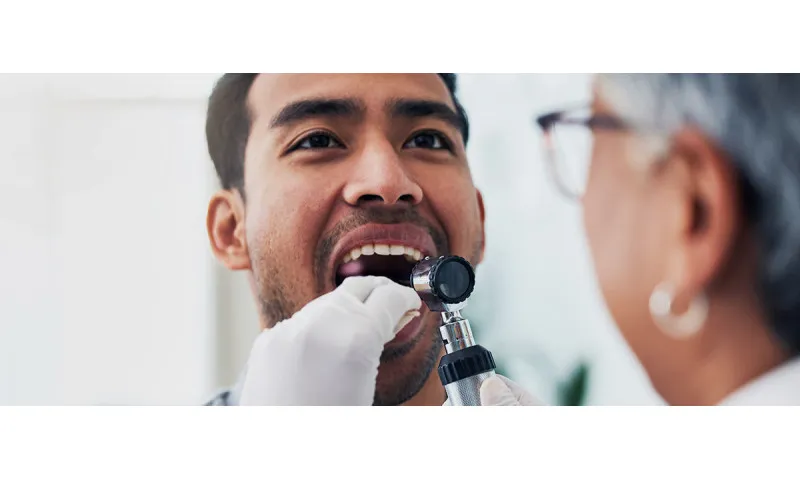
Professional diagnosis: Methods at a glance
The earlier caries is identified, the easier it can be treated. Regular dental check-ups are vital for detecting the early stages of caries. In the following, we will explain how a dentist can identify damage to your teeth that is often invisible to the unprofessional eye.
Dental check-up
The first step in tracking down caries is to closely examine your teeth. To do so, the dentist uses a small mirror and a very bright light. During this initial examination, the dental practitioner can detect changes to the tooth surface that may suggest the presence of caries. If this is indeed the case, the dentist can substantiate their suspicion using a special probe. For instance, if the probe gets caught in a particular area, it typically indicates to the dentist that there is caries present. Since: Healthy tooth enamel is hard and withstands the pressure exerted by the probe. In contrast, once tooth enamel has been compromised by caries, it becomes softer, causing the probe to adhere slightly.
X-ray images
Another tool for detecting even well-hidden caries is an X-ray image. Its big advantage: These images can be used to identify very early stages of damage; a level of detection not possible with a simple probe examination. The drawback, of course, is the exposure to radiation. An X-ray image is usually included in the standard dental check-up, although it is not taken every time to protect a patient's health and safety.
Fibre-optic transillumination (FOTI)
X-ray images and probe-based examinations also have their disadvantages: X-rays expose the body to radiation, and the use of probes carries the risk of potentially damaging the tooth or even transferring cavity-causing bacteria to other teeth. A more gentle approach is fibre-optic transillumination. This method utilises a device to shine light through the teeth. Dentists direct cold light into the tooth using a (blunt) probe. This examination method is particularly well-suited for identifying caries in the interdental spaces of both the posterior and the anterior teeth. The underlying principle: Destroyed tooth substance prevents the transmission of light, resulting in the appearance of a dark spot, indicative of caries.
Electrical resistance measurement using an electric caries monitor (ECM)
Electrical resistance measurement is another method for the early detection of caries. This makes use of the fact that caries changes the electrical resistance of a person's teeth. Healthy tooth enamel has little or no electrical conductivity. However, if it becomes decayed, it loses this insulating property: It starts to conduct electricity. In this case, the resistance between the tooth surface and an electrode decreases.
Laser fluorescence
Diagnostics employing laser fluorescence utilises the fluorescent properties of the tooth structure. Decayed areas exhibit a stronger fluorescence compared to healthy ones. To detect and identify these differences, a specific lamp that emits light at a particular wavelength is used to illuminate the tooth. As a result, caries and the degradation products of the associated bacteria light up in a contrasting colour compared to healthy areas.
Good to know:
Dental check-ups should generally take place at intervals ranging from three to twelve months. Three-month appointments are particularly advisable for individuals with highly susceptible teeth. As standard practice, an interval of twelve months is normal. Children are often scheduled for check-ups every six months.
What to do about caries? This is what caries treatment looks like
Once caries has started, it is crucial to stop the progression of the disease as soon as possible. But how? This also depends on the stage at which the caries is discovered. Find an overview of how to combat the disease below.
Treatment at an early stage – with fluoride against caries
Treatment is most gentle when caries manifests as the "white spots" mentioned earlier. At this early stage of the disease, it is typically unnecessary to employ a dental drill. However, you should not count on self-healing methods either. Without intervention, there is a significant risk of the development of "full-blown caries." Your dentist will probably recommend the use of a high-concentration fluoride toothpaste to promote the remineralisation of the tooth. Multiple fluoride applications may also be suggested as part of the therapy. However, it is just as important to devote even greater attention to meticulous toothbrushing at this stage.
Good to know:
Are you still looking for the ideal toothpaste? Then simply try out the Be You toothpaste series from Curaden. Not only can you select from various flavours like peach, grapefruit, watermelon and even gin tonic, you also receive a toothpaste that effectively provides your teeth with fluoride and features a gentle whitening effect due to the addition of enzymes. And: the added xylitol makes your teeth even more resistant to caries.
Through these relatively straightforward measures, unsightly stains can often be removed. It is important to know, however, that caries does not always manifest as "white spots". Frequently, dentists detect caries during a routine check-up when their patients are completely unaware of its presence. In these cases, the caries is typically at a more advanced stage.
Also important to know: the "white spots" are not always indicative of early-stage caries. Spots on the teeth can also result from a dental injury or excessive fluoride use, with the latter condition being referred to as fluorosis. So, given the multitude of potential causes for white spots on teeth, it is crucial to consult a dentist to receive the appropriate treatment tailored to your specific situation.
Good to know:
White spots can be a first sign of early-stage caries – but they do not necessarily have to be. They may also indicate a condition known as fluorosis. Discover what fluorosis is and what you can do about it in our article:
Treatment of already existing caries
When caries has already reached the dentine, use of a dental drill is often needed. This tool is employed to extract the decayed material from the affected area. The resulting "cavity" must then be filled to restore the tooth's structure. Several materials are suitable for this job, and will be introduced in the following.
Silver amalgam
Silver amalgam comprises silver, mercury, copper, tin and sometimes zinc, palladium or indium. The biggest advantage of this material: It is cost effective and has an average lifespan of 14 years. Moreover, defects are less common with amalgam fillings. Another benefit is that teeth with silver amalgam fillings are less susceptible to secondary caries. The biggest disadvantage, however: Many individuals find the appearance of silver amalgam fillings unattractive. Due to their dark grey (silvery) colour, they stand out prominently from the rest of the tooth. There are also environmental concerns about their mercury content. Because of these aspects, silver amalgam fillings have, in fact, become somewhat outdated.
Composite resins
This type of dental filling is explained as a blend of approximately 20 per cent plastics and around 80 per cent silicic acid salt or fine glass particles. Many patients opt for this type of dental filling because it is tooth coloured, making it blend in seamlessly with healthy teeth or stand out only slightly. In the past, composite fillings had the significant drawback of not being as durable as silver amalgam. Thanks to enhanced material properties and new attachment techniques, this material is now, however, equally as durable.
Composites are initially soft and are hardened using a special blue light lamp after being inserted in the tooth cavity. They need to be bonded to the tooth structure. This is the only way to guarantee that the dental filling stays in place and the tooth achieves its required strength.
Glass ionomer cement
This type of dental filling is a mineral cement designed specifically for use in dental applications. Once the material has hardened, its surface takes on a light and matt appearance. Glass ionomer cement is primarily employed for temporary dental fillings or for treating decayed primary (milk) teeth. Due to its limited life span, this material is not recommended for teeth with chewing surfaces. A special feature of glass ionomer cement: It contains fluoride, which is gradually released into the dental filling. This is done to prevent the formation of caries at the margins of the dental filling.
Compomers
Compomers are a combination of composite and glass ionomer cement. They can be used to treat primary (milk) teeth. Moreover, they can also be used for the necks of teeth and temporary dental fillings. Compomers are not intended for extensive dental fillings in the posterior region of the mouth. The restricted range of application is down to the fact that compomers typically have a lifespan of around three to five years.
Gold foil compaction fillings
This is a rarely used approach for treating caries. With this type of dental filling, the dentist successively "hammers" several layers of very thin gold foil into place in the tooth. The disadvantages are that these dental fillings are rather difficult to produce and the gold colour makes them stand out. The advantage, however, is the durability of the material.
Removing caries without drilling
Many people, old and young alike, are afraid of dental work. Drilling is especially feared. For a long time, patients had no alternative to drilling when it came to caries treatment. Today, this situation has changed – at least in some cases. Treatment without drilling is possible if, for example, the caries is in its early stages, meaning the tooth structure is only minimally affected and the enamel has not yet been impacted. Read about the various possibilities here.
Caries infiltration
With this method (Icon therapy), the decayed surface of the tooth is roughened using a special gel. The decayed parts are thus etched away. This is followed by treatment with Icon, a liquid resin, which fills the gap that has been created. In the process, the resin penetrates deeply into the tooth's vessels and seals them. The dentist then hardens the resin with UV light. This treatment has its limits, however. If parts of the tooth enamel have already been worn away or broken out, a dental filling or inlay will be necessary.
Removal of caries with a laser
A laser can also be used to remove caries from the tooth. This method is particularly effective for accessing hard-to-reach areas in the mouth. The dental laser works like a traditional drill. The dentist points it directly at the caries-affected area and the laser beam removes the diseased parts. Advantages of this treatment method: Laser treatment is painless and quiet. Another benefit: The bright light from the laser can be used to detect caries in its early stages. Caries lesions that were previously imperceptible to the naked eye become visible.
Costs of caries treatment
The costs of caries treatment depend on your health insurance and which country you live in. There are distinct differences here. In Germany: if you have statutory health insurance, you are entitled to a dental filling free of co-payment, which may be amalgam for posterior teeth and composite (plastic) for incisors and front teeth.
For children under 15 and pregnant or breastfeeding women, health insurance funds may also cover the costs of composite fillings in the posterior region. This also applies to dental fillings in milk teeth.
Everything else must be paid for by the patient. A written additional cost agreement is typically required in this case. Obtaining a cost estimate before treatment is important to avoid any unexpected expenses. What many people may also not know: There is a two-year warranty on dental fillings in Germany.
Preventative measures: Preventing caries successfully
The best way to prevent holes in your teeth is good oral hygiene. We have summarised what this entails and how you can enhance your dental health here.
Brush your teeth twice a day
Brushing your teeth in the morning after breakfast and at night before going to bed should be an integral part of your daily routine. If you feel the urge, you can certainly brush your teeth in between, especially after consuming sweet foods and drinks. You should also opt for a toothpaste that contains fluoride. Using a toothpaste with a fluoride content ranging from 1,000 to 1,500 ppm on a daily basis is considered the most effective approach to combating caries. However, it is also crucial to not only clean the easily accessible tooth surfaces but also the spaces between your teeth. For a thorough removal of food debris and plaque, it is best to use interdental brushes.
Good to know:
The Enzycal 950 ppm Fluoride toothpaste from Curaden provides your teeth with the necessary fluoride content. Additional benefit: This toothpaste contains enzymes that naturally occur in saliva, creating a protective shield against cavity-causing bacteria.
Only eat small amounts of sweet food items
Cavity-causing bacteria love sugar. They convert it into acid, which then attacks the tooth enamel. That is why you should limit your consumption of sugary foods. Ideally, eat sweets immediately after a meal and then brush your teeth thoroughly. It is not at all advisable to let your teeth come into contact with sugar throughout the day – for example, with apple juice or other fruit juices. As you are basically rinsing your teeth with sugar.
Xylitol against caries: Chewing gum helps!
Chewing gum has the advantage that it helps prevent caries: It stimulates the flow of saliva and thus neutralises harmful acids more quickly. So, by regularly chewing sugar-free gum after eating or drinking, you can lower your risk of caries. It is recommended to choose chewing gum containing xylitol, such as the Black is white chewing gum from Curaprox. This sugar substitute has proven effective in reducing plaque formation and the production of acids that can damage teeth.
Regular check-ups and professional dental cleaning
Since caries likes to develop out of sight at first, it is important to visit a dentist regularly, even if you do not have any symptoms. It is also a good idea to make an appointment for a professional dental cleaning procedure at least once a year. Dental hygienists remove stubborn plaque and especially tartar that can no longer be removed with a toothbrush alone.
Fissure sealing
Our chewing surfaces are never smooth and even; they are filled with fissures, grooves and crevices. These areas are particularly vulnerable to caries because they are harder to clean. Erupting teeth, especially in children and teenagers, are at particular risk and might benefit from fissure sealing. With this sealing method, the dentist seals the fissures with a special material – usually plastic. This prevents bacteria from reaching the chewing surfaces.
Additional fluoride administration, if necessary
During dental check-ups, your dentist will determine whether it might be beneficial in your specific case to incorporate fluoride through varnishes, rinsing solutions or gels in addition to the fluoride toothpaste you use at home. For instance, in patients susceptible to root caries, quarterly treatment with fluoride varnish has been demonstrated to decrease caries. In Germany, it is recommended to apply a fluoride varnish twice a year for children and teenagers.
Good to know:
Not only adults, but also babies and young children can develop caries. In fact, as soon as the first milk tooth comes through. That is why dental care is so important from the very first milk tooth. The Curaden baby toothbrush makes brushing your child's teeth especially pleasant and easy.
Chlorhexidine varnish, if necessary
Erupting permanent teeth can receive added protection through chlorhexidine varnishes with a minimum concentration of one per cent. This type of application can also be useful in the area of exposed root surfaces. Have a word with your dentist to find out whether this kind treatment makes sense for you.
Healing caries naturally? Not a chance
Wondering whether you can heal caries yourself? Unfortunately, the answer is: No. Cavities in the tooth must be addressed professionally. Attempting to do it yourself can cause significant damage to your teeth and leave you in significant pain.
When experiencing toothache, there are a few home remedies that might provide some relief. These include sage tea, crushed onions as a compress or clove oil. But they should not be relied upon as a cure. The first priority should, therefore, always be to go and see your dentist.
Sources
André Melchior, Doctor Melchior & Team Zahnärzte im Mediapark: Loch im Zahn: Symptome, Behandlung und Vorbeugung.
AWMF-Leitlinie: Kariesprophylaxe bei bleibenden Zähnen – grundlegende Empfehlungen, dated: 2021.
Deutsche Familienversicherung:
Kariesinfiltration: Die Kariesbehandlung ohne Bohren, dated: 2019.
Laserbehandlung beim Zahnarzt, dated: 2019.
Deutsche Gesellschaft für Zahnerhaltung: Sieben grundlegende Empfehlungen zur Kariesprophylaxe bei bleibenden Zähnen.
Gesellschaft für Zahngesundheit, Funktion und Ästhetik: Erosionen: Schädigungen der Zahnhartsubstanz durch Säuren.
Hennessy, Bernard J.: Karies / Pulpitis, at: msdmanuals.com.
German National Association of Statutory Health Insurance Physicians
Lussi, Adrian: Karies unter Strom, at: spektrum.de.
Praxis für Zahngesundheit, Kuroszczyk, Dagmar und Dr. Andrzej: Kompomere und Komposite: Zahnfarbene Kunststofffüllungen, dated: 2023.
Universität Zürich: Genetische Defekte im Zahnschmelz begünstigen die Bildung von Karies.
Federation of German Consumer Organisations: Karies: Welche Kosten übernimmt die Krankenkasse?.
ZWP Online: Diagnostik in der Karies- und Parodontitisprophylaxe.
Zahnfüllungen: Kunstharze als bevorzugtes Material.
All websites last accessed on 3 September 2023
 Swiss premium oral care
Swiss premium oral care