The most important facts in brief
- Definition: Tongue cancer is a malignant tumour in the tongue area and a subtype of oral cavity cancer.
- Prognosis: The earlier tongue cancer is detected, the higher the chances of recovery. If detected at an early stage, the five-year survival rate is 80 per cent; depending on the location, the average is 15 to 50 per cent.
- Symptoms: The first signs include red or white patches (leukoplakia) on the tongue, sores and a foreign body sensation.
- Causes: Smoking, frequent alcohol consumption, an unbalanced diet, poor oral hygiene and HPV viruses are among the most common risk factors.
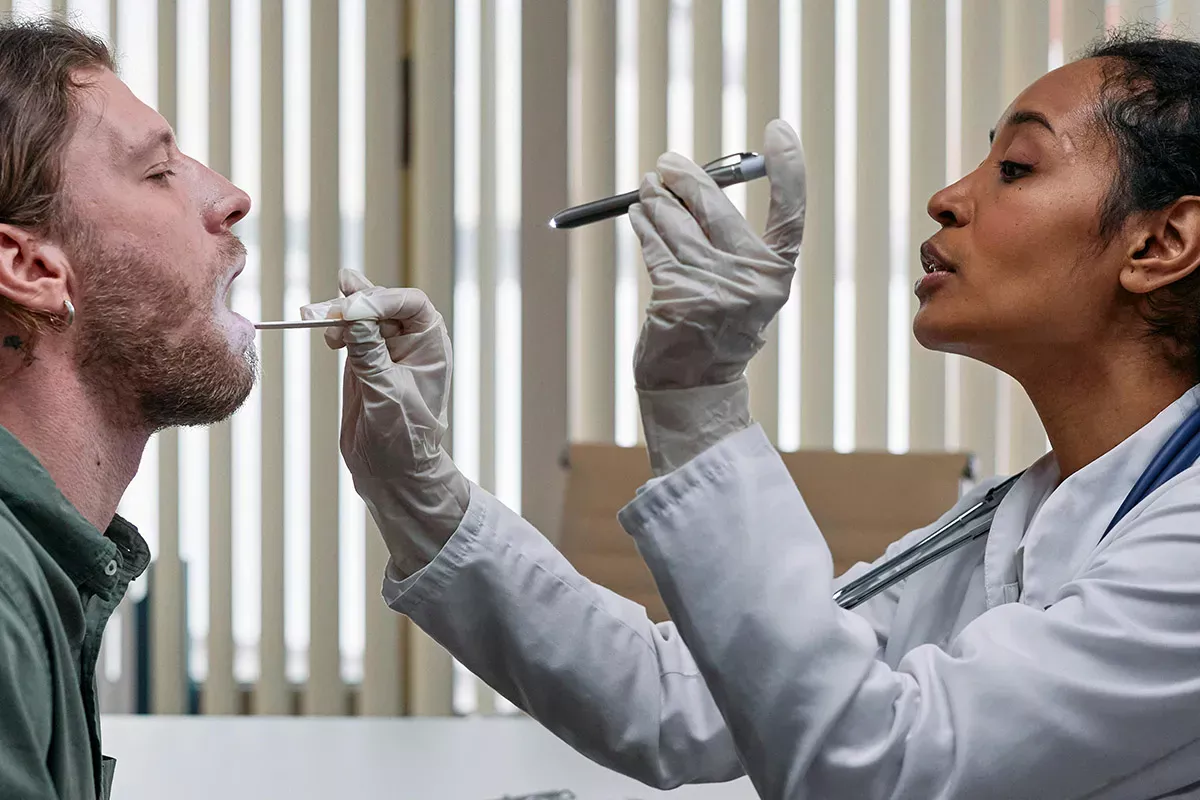
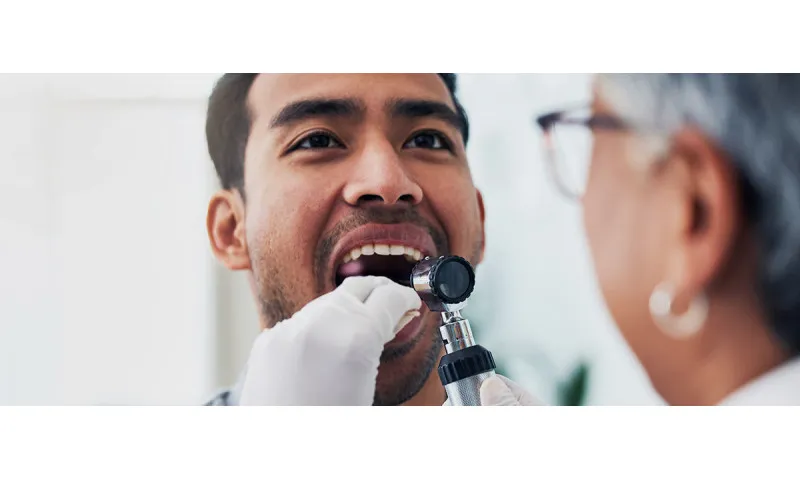
- Diagnosis: The doctor takes a tissue sample to determine whether a tumour is present. This is followed by imaging procedures such as MRI, CT, ultrasound or X-ray.
- Treatment: If possible, the tumour is surgically removed in the case of tongue cancer. This can be followed by radiotherapy, chemotherapy or immunotherapy - a combination is also possible.
- Prophylaxis: If you want to protect yourself against tongue cancer, you should stop smoking and regular alcohol consumption, pay particular attention to thorough oral hygiene and attend dental check-ups.
Good to know:
This article deals with the specifics of tongue cancer, a subtype of oral cavity cancer. You can find more detailed information, especially on diagnosis and treatment, in our main article "What to do about oral cavity cancer?"
Definition: What is tongue cancer?
Tongue cancer (technical term: tongue carcinoma) is a malignant tumour in the tongue area and falls into the category of oral cavity cancer. Tongue cancer is particularly common on the front two-thirds of the tongue - either on the side, directly on the tongue or on the underside of the tongue. Tumours under the tongue are usually cancer of the floor of the mouth and not tongue cancer. If tongue cancer develops far back on the last third of the tongue, it can also be referred to as throat cancer.
In around 95 per cent of cases, tongue cancer originates from the uppermost layer of the oral mucosa, the squamous epithelium. Tongue cancer can metastasise to the lymph nodes and also spread to other organs via the bloodstream, where it can impair vital functions.
Good to know: What exactly is cancer?
Cancer develops when normal cell renewal is out of balance. Cancer cells with altered genetic information are not recognised by the immune system and spread faster than normal cells. As a result, healthy cells are displaced and the tumour grows. It becomes dangerous when the cancer cells spread through metastases in the body and affect vital organs.
Frequency of tongue cancer
In the oral cavity cancer category, tongue cancer is one of the most common forms of cancer. However, as the statistics do not differentiate between the various types of oral cavity cancer, no exact figures are available. Between 200,000 and 350,000 people worldwide are diagnosed with oral cavity cancer every year - around 12,000 in Germany and 1,200 in Switzerland, and the trend is rising.
This increasingly affects people who do not fall into the main risk group of men over the age of 65 who smoke and regularly drink alcohol. This group still accounts for two thirds of those affected. However, women and younger people are also increasingly affected by tongue cancer - some as young as 20 or 30. Tongue cancer is very rare in children.
Prognosis: Can tongue cancer be cured?
In the case of cancer, life expectancy is usually expressed as a "five-year survival rate". This value indicates the percentage of patients who are still alive five years after the start of treatment.
The chances of curing tongue cancer depend heavily on the stage at which the cancer is diagnosed, the size of the tumour and whether metastases have already formed. If the tumour is detected at an early stage, the chances of recovery are very good. The five-year survival rate is up to 80 per cent. The later the tongue cancer is diagnosed, the lower the probability that the tongue cancer will be cured.
In addition to the size of the tumour at the start of treatment, the location is also decisive: the five-year survival rate for tumours on the edge of the tongue is between 35 and 50 per cent. For tumours on the base of the tongue, the rearmost part of the tongue, only 15 to 25 per cent of patients are alive five years after the start of treatment. The general state of health of the person affected also plays a major role in life expectancy.
Good to know:
After being diagnosed, many people find it helpful to read or watch testimonials from people who have already overcome tongue cancer and talk about their experience with tongue cancer surgery and other forms of treatment. This also helps with a realistic assessment of what to expect during treatment. Self-help groups and social organisations can also offer support. You can find more information on this in the patient guidelines for oral cavity cancer.
Symptoms: How do you recognise tongue cancer?
Tongue cancer goes through several stages, from the preliminary stage to the first signs to the fatal final stage. The cancer often remains unrecognised for a long time as it does not cause any pain in the early stages. Here you will find lists of symptoms as well as images of the preliminary stage, initial stage and advanced stage.
Leukoplakia: Possible precursor of tongue cancer
Leukoplakia is a change in the mucous membrane of the tongue: Cornifications form on the uppermost layer of the tongue mucosa, which swell due to the moist environment in the mouth and turn white in colour. The result: white patches on the tongue. The causes of leukoplakia are injuries to the mucous membrane, poor oral hygiene, smoking, alcohol consumption, an unhealthy diet and viral or fungal infections.
Leukoplakia is usually harmless if it is treated. However, if left untreated, it can develop into tongue cancer. An estimated 30 percent of untreated leukoplakia can develop into a malignant tumour. You should therefore take white spots on the tongue seriously and have them examined by a doctor.
First signs of tongue cancer
In the early stages, tongue cancer often goes unnoticed. It is therefore important that you take every little "ache" in the tongue area seriously. After all, it could be the first sign of tongue cancer.
The following symptoms are possible in the initial phase:
- White or reddish spots on the tongue
- Sore spots on the edge of the tongue or on the underside of the tongue
- Stinging or burning
- Foreign body sensation/numbness
- Bleeding in the tongue area (without prior injury to the mucous membrane)
- Increased salivation
- Bad breath
Good to know:
In some medical conditions, such as heart attacks or strokes, the first signs differ between men and women. This is not the case with tongue cancer. According to current research, the symptoms in women and men are the same.
Advanced stage
The growth of the tumour causes further tongue cancer symptoms:
- Painful ulcers
- Hardened bumps/nodes
- Swelling of the tongue
- Swallowing difficulties
- Speech problems
- Sore throat that radiates to the neck, lower jaw and ears
- Restricted mobility of the tongue
- Swollen lymph nodes
The appearance of the tumours can vary: There are flat and also cauliflower-like tumours. Several individual tumours are also possible.
In addition, general symptoms of malaise often occur:
- Tiredness
- Fatigue
- Loss of appetite
- Weight loss
- Concentration difficulties
- Poor performance
- Fever spikes and night sweats
Does tongue cancer hurt?
The tumour ulcer that forms as a result of tongue cancer is often painful in its advanced stages. It can also lead to painful swallowing difficulties and a sore throat.
Metastases: Where does tongue cancer spread to?
At an advanced stage, tongue cancer spreads to the surrounding tissue via the lymph nodes. This can lead to the formation of metastases in the lower jaw area, for example. However, it is even more dangerous if the cancer spreads throughout the body via the bloodstream or lymph nodes and forms distant metastases in vital organs. The liver, bones and brain are particularly frequently affected.
End stage: Fatal course
Regardless of the size of the actual tumour, the final stage of tongue cancer is reached when vital organs are affected and will no longer be able to fulfil their function in the foreseeable future. The body and the immune system are increasingly weakened and a cure is no longer possible.
In addition, people with tongue cancer are often unable to eat properly in the final stages and therefore lose a lot of weight.
Causes: Where does tongue cancer come from?
The exact causes of tongue cancer have not yet been clarified. However, there are a number of risk factors that favour the development of cancer:
- Smoking (cigarettes or e-cigarettes)
- Frequent alcohol consumption (especially high-proof alcohol in combination with tobacco consumption)
- Infection with human papillomavirus (HPV), Eppstein-Barr virus and other viruses
- Poor oral hygiene
- Chronic inflammation of the mucous membranes
- Inflammation at the edge of the tongue due to ill-fitting dentures
- Unbalanced diet with nitrite-containing foods (e.g. sausage and cured meat)
Good to know: Is tongue cancer contagious?
No, tongue cancer is not contagious. However, it should be noted that some viruses are considered a risk factor and are indeed contagious. Human papillomaviruses, for example, are primarily known to cause cervical cancer and can be transmitted through oral sex. They are considered the main cause of oral cancer in people under 30. Children and adolescents can now be vaccinated against HPV.
Diagnosis: Choice of doctor for tongue cancer
If you suspect you have tongue cancer, you should have a medical check-up as soon as possible. After all, the chances of recovery are much better if you start treatment as early as possible.
Which doctor for tongue cancer?
The first port of call is your family doctor. During the initial examination, a tissue sample will be taken from the affected area to determine whether it is actually a tumour or not. If necessary, your dermatologist d will refer you to an ENT specialist or oncologist - a cancer specialist. In addition, imaging procedures such as computer tomography (CT), magnetic resonance imaging (MRI), ultrasound and X-rays can be used to determine the severity of the tumour. However, blood tests do not provide any information about a possible tongue cancer.
If the suspicion of tongue cancer is confirmed, treatment is carried out by a team of experts with representatives from all relevant medical specialities. You can find more detailed information on the diagnosis and classification of the tumour in our article on oral cavity cancer.
Good to know:
Because tongue cancer tends to be inconspicuous in the early stages, the dentist often recognises tongue cancer first. During a check-up, dentists not only examine the teeth, but usually also the tongue and gums. ENT specialists or orthodontists can also detect signs of tongue cancer during an examination.
Treatment of tongue cancer
The treatment depends on how advanced the tongue cancer is, where it is located and whether metastases have already formed. Here we only briefly describe the possible treatment methods. Further information and details on the side effects of radiotherapy, immunotherapy and chemotherapy can be found in our main article on oral cavity cancer. The German Cancer Aid's Blue Guide and the oral cavity cancer patient guidelines are even more comprehensive. There you will also find important information about patients' rights.
Tongue cancer is usually treated with surgery to remove the tumour. In order to prevent a recurrence, radiotherapy, immunotherapy or chemotherapy or a combination of these methods can then be used. In some cases, tongue cancer tumours cannot be removed surgically due to their location or size. A combination of radiotherapy and chemotherapy is then usually used.
The treatment is followed by a stay in a rehabilitation clinic and regular follow-up checks in order to detect a possible recurrence - a new formation of the tumour - at an early stage.
Surgery for tongue cancer
The aim of the operation is to completely remove the tumour from the tongue while preserving tongue function as much as possible. This is often relatively easy to achieve in the front part of the tongue. More complex procedures are required for tongue cancer on the back part of the tongue. During the operation, the surgeon often removes part of the healthy tissue as well as the tumour tissue, as there may be small, invisible outgrowths around the tumour. If metastases have already formed in the lymph nodes of the neck or are suspected, the surgeon will also remove these. The operation can be performed using a laser.
If large parts of the tongue are removed during surgery and this could impair speech, chewing or swallowing function, the surgeons reconstruct the tongue to restore its original shape. To do this, they remove tissue from another part of the body - such as the forearm - and reattach it to the tongue. In this way, function and appearance can be preserved. However, those affected must be prepared to get used to the new tongue first, which can be a months-long process.
Challenges after tongue cancer treatment
The tongue is an important organ of the body. Without it, we cannot speak or swallow. The taste buds are also located on the tongue. During cancer treatment, these important functions can be severely restricted as a result of surgery or radiotherapy. The aim of treatment is therefore not only to remove the tumour, but also to maintain or restore tongue function. Tongue cancer patients may face the following challenges after successful cancer treatment:
Learn to speak again
If parts of the tongue are removed during tongue cancer surgery, speech may be impaired. The voice often sounds softer and somewhat hoarse and certain words can be difficult to pronounce. The symptoms can be temporary or permanent. Speech therapy can help those affected to restore their ability to speak.
Learn to eat again
The swallowing function also poses major challenges for tongue cancer patients and must be trained. A feeding tube may be used temporarily during cancer treatment. Soft foods such as soups, porridge and yoghurt are particularly suitable for getting used to eating again after treatment. If the oral mucosa is inflamed, patients should avoid acidic foods such as citrus fruits or hard foods such as crisps. Instead of the usual three main meals, several small meals are recommended.
Good to know:
Cancer treatments often lead to inflammation of the oral mucosa and the wound is also very sensitive after the operation. The CS Surgical toothbrush with particularly soft bristles offers gentle cleaning for freshly operated or inflamed mouths. An antibacterial mouthwash with chlorhexidine can also be useful to protect against inflammation. The Perio plus Regenerate mouthwash from Curaprox also supports wound healing and contains a natural extract of bitter orange to enhance the effect of chlorhexidine.
Change in the sense of taste
Tongue cancer surgery not only removes the tumour, but also some of the taste buds. So it's no wonder that some foods taste different after treatment than before. This change is irreversible. It's best to simply try out what you like and don't like with your new sense of taste.
Dry mouth
Patients often complain of persistent dry mouth, especially after radiotherapy. It is best to always have a bottle of water to hand and also consume plenty of fluids with food in the form of soups and soft foods. Sugar-free lozenges can also help. In our article on the topic of Dry mouth you will find numerous other tips on how to get rid of the feeling of dryness.
Good to know:
Dry mouth is not only unpleasant, but actually dangerous for your teeth because the caries-protecting effect of saliva is missing. This is why thorough oral hygiene is particularly important in the case of dry mouth. To stimulate saliva production, you can chew sugar-free chewing gum or use a saliva-promoting toothpaste. The toothpastes in the Enzycal range from Curaprox contain three enzymes that also occur naturally in saliva and therefore protect your teeth and stimulate the flow of saliva.
Prophylaxis: How you can prevent tongue cancer
Even if it is not yet clear what is ultimately the decisive factor for the development of cancer, you can eliminate some of the risk factors and thus ensure that the likelihood of developing tongue cancer is significantly reduced.
Stop smoking and drinking alcohol
Excessive alcohol and tobacco consumption is the number one risk factor for oral cavity cancer. People who smoke and regularly consume high-proof alcohol are 30 times more likely to develop cancer of the oral cavity than non-smokers who do not drink regularly. Therefore, the most effective protection against tongue cancer is to stop smoking and drinking. This will also make you less susceptible to all other types of oral diseases - including tooth decay and periodontitis. Your liver and lungs will also thank you if you switch to a healthy lifestyle.
Regular check-ups
As tongue cancer is often detected "by chance" by the dentist, it is important that you attend regular check-ups. After all, if tongue cancer wants to spread in your mouth, it will have a much worse chance if you discover it at an early stage. Some dental practices also offer a special early detection examination.
Important: If you wear dentures, you should also have them checked regularly to make sure they fit properly and have them relined if necessary. This will help you avoid pressure points and skin irritation, which can become inflamed and are also a risk factor for tongue cancer.
Examine your tongue regularly
After brushing your teeth, simply stick your tongue out wide and examine it from all sides for any abnormalities. This could be stains, discolouration or growths, for example. Move your tongue to the left and right so that you can inspect the sides. Finally, lift the tongue so that you can also examine the underside.
Ensure good oral hygiene
Poor oral hygiene is also a risk factor for tongue cancer. Good and thorough oral hygiene includes the following points:
- Brush your teeth twice a day - after breakfast and before going to bed
- Clean interdental spaces once a day with an interdental brush
- Clean tongue once a day with tongue scraper
You can find out exactly how to use the respective aids and what the most efficient brushing technique is according to current research here:
Instructions: Brush your teeth properly
Instructions: Brushing your teeth properly with an electric toothbrush
Good to know:
Many people make the mistake of using a toothbrush that is too hard when brushing their teeth. In fact, a soft toothbrush has a much more thorough cleaning power and is much gentler on the gums. Curaprox toothbrushes are recommended by dentists all over the world because, thanks to a particularly dense bristle head with up to 12,460 bristles, they can tackle plaque much more thoroughly than conventional toothbrushes with an average of 500 bristles.
Sources
Braunstein, Claudia: My life eight years after being diagnosed with tongue cancer, on: geschmeidigekoestlichkeiten.de.
German Cancer Aid: Cancer in the oral and maxillofacial region (The blue guides).
German Cancer Research Centre (DKFZ): How do metastases develop?
D'Souza, G. et al: Understanding personal risk of oropharyngeal cancer: risk-groups for oncogenic oral HPV infection and oropharyngeal cancer, in: Annals of Oncology. 2017.
Gently: How to manage the dental treatment of the oncology patients?
Gesellschaft für Sexualwissenschaft e.V.: Oral sex can trigger tumours in the mouth and throat area.
Gesundheit.gv.at (Austrian public health portal): Tongue cancer.
Högemann, Astrid et al: Tongue carcinoma, at: flexikon.docchceck.com.
Kahle, Charly: Tongue cancer, on: meine-gesundheit.de
Lang, Carina: Tongue cancer (tongue carcinoma): Signs and treatment, on: gesundheit.de.
Oncology guideline programme (Association of the Scientific Medical Societies in Germany (AWMF), the German Cancer Society (DKG) and the German Cancer Aid Foundation(: Patient guideline for oral cavity cancer.
Oncology guideline programme: S3 guideline on the diagnosis and treatment of oral cavity carcinoma.
Let's Talk about Mouth Cancer: #mouthcheck.
Morisch, Susanne: Metastases, on: journalonko.de.
NetDoktor: Tongue cancer.
Rühl, Ramona: Krebsstadien: Verlauf, Stadien & Krebstod, on: pflege.de.
University Hospital Zurich (USZ): Leukoplakia.
All websites last accessed on 21/07/2023.
 Swiss premium oral care
Swiss premium oral care