Oral leukoplakia: What is it?
The clinical picture of oral leukoplakia is characterised by a whitish change in the oral mucosa. This change appears in the form of small or large white patches. These symptoms gave the disease its medical name: "leukos" means "white" in Greek and "plakos" means "plate". The disease is also known as "white callus disease".
It is important to know that the disease should not be taken lightly. Although the whitish coating can be harmless, it can also develop into oral cancer.
But where does the whitish coating in the mouth actually come from? It is usually caused by a "disruptive factor" that irritates the oral mucosa. The main risks for the outbreak of leukoplakia are smoking and the consumption of alcohol and chewing tobacco. However, ill-fitting dentures or braces can also damage the mucous membrane. In these cases, this leads to excessive cell production and/or abnormal cell development in the oral cavity. As a result, the uppermost tissue layer of the oral mucosa becomes keratinised. The moist environment in the mouth then causes the keratinised cells to swell, causing them to become whitish in colour and thicken. Oral leukoplakia is therefore caused by stimuli - and not by viruses or bacteria. As a result, it is also not contagious.
Where can leukoplakia occur?
In principle, the whitish patches can appear anywhere in the oral cavity. However, they are particularly common on the mucous membranes of the cheek, on the tongue and on the floor of the mouth.
The following areas may also be affected:
- Lip
- Gums
- Palate
- Throat
However, leukoplakia can also occur in other parts of the body with mucosal tissue - for example in the genital area ( vagina, vulva, clitoris, glans, foreskin).
Other parts of the body that can be affected are:
- Urinary bladder
- Vocal cords
- Eyes (conjunctiva)
- Anus (anal mucosa)
Frequency : How many people are affected by oral leukoplakia?
In Germany, around 2.3 per cent of all men and 0.9 per cent of all women are affected by oral leukoplakia. The disease is most common in men from middle age onwards - an onset before the age of 40 is rare.
Different types of leukoplakia
Leukoplakia is divided into three different types, which we would now like to introduce to you:
Homogeneous (uniform) leukoplakia
In this form of leukoplakia, the affected mucosa is white throughout, has a smooth surface and a sharp demarcation to the healthy area. Homogeneous leukoplakia is also known as simple leukoplakia.
Verrucous (warty) leukoplakia
With verrucous leukoplakia, the surface of the affected oral mucosa is rough and wart-like. Those affected often also notice a burning sensation or experience pain. This type of leukoplakia belongs to the so-called inhomogeneous (not evenly structured) leukoplakia.
Erosive leukoplakia
This type of leukoplakia is characterised by red and white discolouration with irregular boundaries. Here it is characteristic that more and more red areas gradually form on the mucous membrane. The white discolourations, on the other hand, recede into the background. This type of leukoplakia also belongs to the inhomogeneous, i.e. not evenly structured, forms.
Special form: Oral hair leukoplakia
In this particular form of leukoplakia, the whitish changes appear on the sides of the tongue. They resemble small hairs in appearance. Oral hair leukoplakia can occur in people with an HIV infection. It is triggered by an infection with the Epstein-Barr virus (Pfeiffer's glandular fever). Antiviral drugs can combat this form of leukoplakia.
Good to know:
The counterpart to a leukoplakia is the erythroplakia. This is a hardened lesion of the mucous membrane with dark red discolouration. This condition leads to cancer more frequently than leukoplakia.
Causes and risk factors for oral leukoplakia
There are a number of causes that can be behind oral leukoplakia. We present them to you in detail here.
Cigarette and alcohol consumption
People who smoke and drink alcohol have a particularly high risk of damaging the cells of the oral mucosa and developing leukoplakia. In the worst case scenario, this is a precancerous condition. If the leukoplakia remains untreated, a carcinoma of the oral cavity can gradually develop.
Good to know:
Oral leukoplakia can develop into oral cancer. You can find out exactly what this disease is, how to recognise it and how it can be treated here:
Mechanical irritation
If braces, poorly fitting dentures or even protruding teeth permanently irritate the oral mucosa, leukoplakia can also develop. Even nails clamped between the lips can contribute to this - at least if this happens repeatedly, for example during manual labour.
Poor oral hygiene and tooth decay
People who do not brush their teeth regularly and sufficiently not only risk cavities, but also the formation of leukoplakia.
Good to know:
Would you like to take a closer look at your oral hygiene and are wondering how to brush your teeth sufficiently and effectively? We have written this down for you in detail in this article:
Unhealthy diet
If a poor diet leads to a vitamin deficiency (A and B vitamins) or iron deficiency, this also increases the likelihood of unsightly white spots developing in the mouth.
Viruses and fungi
An infection with viruses and fungi can also trigger leukoplakia.
Good to know:
If none of the causes mentioned are behind leukoplakia, it is referred to in medicine as idiopathic leukoplakia.
Diagnosis: Recognising oral leukoplakia
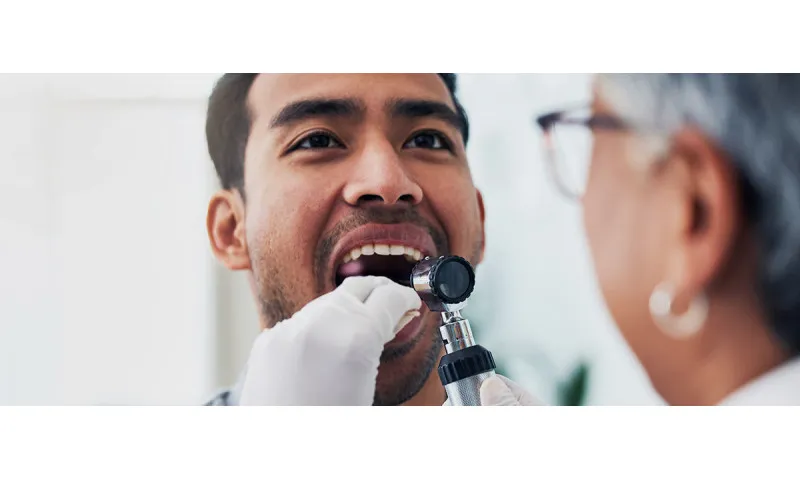
First of all, the question: Which doctor is the right person to contact if you have any abnormalities in your mouth? In principle, you can choose between a dental practice and an ENT practice. Sometimes, however, this question is unnecessary because dentists notice changes during routine check-ups that the patient has not even noticed.
If changes in the mouth give rise to the suspicion of leukoplakia, the doctor will examine and palpate the affected area in detail. If the area shows typical white patches and these cannot be wiped off, it is reasonable to assume that the disease in question is present. In addition, the doctor will use a diagnosis of exclusion to differentiate your symptoms from other causes of the disease - as oral leukoplakia can resemble fungal disease such as thrush at first glance. If the white patches persist for two to four weeks, the suspicion of oral leukoplakia is already very clear.
For final certainty, a tissue sample is then taken from the affected mucosa by means of a biopsy. Analysing the cells in the laboratory then clarifies whether it is actually a leukoplakia - and whether it is already a precancerous stage or still harmless.
Good to know:
If a tissue sample reveals that your oral leukoplakia is already a dangerous precancerous stage, this can be a shock. Perhaps it will help you to share experiences with other people affected? You can find many forums on the subject on the Internet.
And another important tip: try to avoid self-diagnosis - even if it's difficult not to google your own symptoms; we've probably all done that at some point. However, oral leukoplakia must always be diagnosed by a doctor. Pictures on the internet can be misleading. White plaque in the mouth in particular can also have other causes and indicate a wide variety of diseases - for example, a fungal infection in the mouth.
Oral leukoplakia: Prognosis
Those affected naturally ask themselves what the chances of a cure for leukoplakia are. Firstly, it can be said that in many cases the disease can disappear on its own. However, the causes must be eliminated. This means that if, for example, braces or poorly fitting dentures are to blame for the disease, it may well be that the whitish coating disappears as soon as the irritation in the mouth no longer exists. This also applies if high tobacco and alcohol consumption is responsible for the disease - and both are no longer consumed by the patient. In such cases, there is a good chance that the disease will be over after around four weeks.
If the white area in the mouth does not disappear by itself disappears, it should be treated. This is because even if a biopsy shows that the whitish patches are harmless, they can still develop into a precancerous condition at any time. It is estimated that up to 30 percent of untreated leukoplakia will develop into a tumour at the affected site - a so-called squamous cell carcinoma.
And: even if an oral leukoplakia has been removed, there is a high risk that it will reappear. It is therefore important to know the risk factors and causes, avoid them as far as possible and have your mouth checked regularly for new formations. You can read about the best ways to prevent oral leukoplakia in the section "Preventing oral leukoplakia: how to take the right precautions".
Treating oral leukoplakia: Therapies at a glance
The type of treatment for oral leukoplakia always depends on the cause. As you have already learnt above, the first step is to remove the stimulus that is responsible for the white spots - be it dentures or braces, alcohol or cigarette consumption. If the cause is unknown or the oral leukoplakia is already advanced, a doctor usually has to remove it surgically. There are several options available here:
- Excision: the classic cutting out
- Curettage: scraping off the white areas
- Electrosurgery: cutting out with high-frequency current
- Cryosurgery: destruction of tissue through freezing
- Laser surgery
Classical excision is usually the method of choice. It offers the advantage that the diseased tissue can then be pathologically analysed in the laboratory. This makes it possible to determine whether the disease is malignant or not. In addition, excision also allows a larger area of surrounding healthy tissue to be removed to ensure that no malignant cells remain.
Home remedies for leukoplakia?
You should always consult a doctor and have yourself examined if you notice any changes in your mouth. Only a doctor can tell you whether the change is a leukoplakia and what you should do about it.
Nevertheless, you can also try to support the healing process yourself - with green tea. There are studies that suggest that this type of tea has a positive effect on the diseased oral mucosa and reduces the risk of oral cancer. Researchers suspect that the positive effect can be attributed to the fact that the extracts in green tea inhibit the development of new blood vessels - which is necessary for cancer growth. You don't even have to drink green tea to achieve this effect. You can also simply use it as a mouthwash.
So while green tea does indeed appear to have a positive effect on oral leukoplakia, there is no such evidence for homeopathy and naturopathy. You should therefore never rely on these treatment methods and should always seek conventional medical treatment.
Preventing oral leukoplakia: how to take the right precautions
You now know that many oral leukoplakia are caused by a disruptive factor that irritates the oral mucosa to such an extent that it becomes diseased. The most effective way to prevent leukoplakia is therefore to eliminate these irritating factors. Here we explain in detail what you can do to care for your oral mucosa and keep it healthy.
Avoid alcohol and cigarettes
Smokers are particularly at risk of developing oral leukoplakia. If they also consume alcohol, the risk increases considerably. So try to avoid both as much as possible to protect not only your oral cavity but also your whole body.
Good to know:
Cigarette consumption can not only cause serious illnesses such as cancer and cardiovascular diseases. Less dramatic, but unattractive to look at, are the visual changes - such as yellow teeth. We have summarised what you can do about it here:
Tooth discolouration: Where it comes from and how it disappears
Ensure very good oral hygiene
Studies have proven this: Inadequate dental care increases the risk of cancer in the oral cavity and the development of oral leukoplakia. So brush your teeth very well and also use interdental brushes and dental floss to reach the spaces between your teeth. It is also very important to attend regular check-ups at the dentist and to have your teeth professionally cleaned once a year.
Good to know:
Pathogenic caries bacteria like to make themselves at home in the hard-to-reach interdental spaces. With Curaprox interdental brushes, you can remove them quickly and effectively. One application per day is sufficient.
Eat a varied and balanced diet
As you have already learnt, a nutritional deficiency is also one of the risk factors in the development of oral leukoplakia. So make sure you eat a healthy diet. Roughly summarised, this means: Eat plenty of fruit and vegetables, enjoy dairy products and stay away from meat and sausage products. You should also limit your sugar intake. This also kills two birds with one stone, as sugar consumption also leads to a higher risk of tooth decay.
Remain mindful of changes in the mouth
If something changes in your mouth, you should always consult a doctor. This is especially true if you cannot avoid the risk factors for oral leukoplakia already mentioned and are a smoker, for example. Remain vigilant even if you have already had oral leukoplakia and it has been removed. Unfortunately, there is still a risk that it will form again.
Do not accept any disruptive factors in the mouth
The braces pinch here and there? The fixed brackets sting? Or the prosthesis doesn't fit comfortably? These are all reasons to go to the doctor. Some people have been putting up with their unpleasant oral problems for years - this is not only unnecessary, but can be dangerous. As you know, the permanent irritation caused by this can trigger oral leukoplakia and thus increase the likelihood of oral cancer.
Good to know:
It is important to recognise and treat oral leukoplakia at an early stage. The oral cavity cancer that may develop as a result can drastically reduce life expectancy : the five-year survival rate is only 50 per cent - which is mainly due to the often late diagnosis. If the cancer is detected early, however, the survival rate is 90 per cent.
Sources:
AWMF online: S3 guideline Diagnostics and therapy of oral cavity carcinoma.
Federal Ministry of Health: N88.0: Leukoplakia of the cervix uteri.
Deutsche Apotheker Zeitung: Green tea protects against oral cancer.
Deutsche Gesellschaft für Dermatochirurgie e.V.: Operation techniques.
German Society of Oral and Maxillofacial Surgery: Oral leukoplakia/erythroplakia.
German Cancer Research Centre: Smoking and oral health.
DocCheck Flexicon: Cryosurgery.
Ebhardt, Dr med Harald et al: Leukoplakia of the oral mucosa: Diagnostics - Therapy - Prognosis at: epaper.zwp-online.info.
Free Clinics Bremen: When the hoarseness won't go away.
ENT doctors on the net: Green tea protects against oral cavity cancer.
Initiative proDente: Leukoplakia: What influence does smoking have?
Krebsinformationsdienst: Cancer risk and oral hygiene: Brushing your teeth protects you.
MKG Chirurgie Hamm: Oral mucosal diseases.
Springer-Verlag Berlin Heidelberg: Urinary tract infection - leukoplakia of the urinary bladder.
Springer Medizin Verlag: Leukoplakia of the lower tarsal conjunctiva.
University Hospital Düsseldorf: Oral mucosal diseases.
University Hospital Zurich: Leukoplakia.
Science news: Green tea extract for cancer prevention?
ZWP online: Treatment of oral leukoplakia and malignant oral mucosal lesions.
All websites last accessed on 8 April 2024.
 Swiss premium oral care
Swiss premium oral care