What is an abscess?
Abscesses are an encapsulation of pus that builds up within tissue. They occur, for example, in the oral cavity, but also in many different parts of the body, such as the abdomen, internal organs and even on the face. An abscess in the throat is also possible.
Generally speaking, abscesses should never be taken lightly: If the collection of pus spreads inwards deeper into the skin, the highly infectious pathogens also spread beyond the tissues and into the bloodstream. Abscesses, if left untreated, can affect the nerves and muscles and eventually cause permanent brain damage. Furthermore, blood poisoning is a real possibility. An abscess is therefore a potentially life-threatening problem that requires medical treatment.
How does an abscess form?
In most cases, an abscess is caused by a bacterial infection that enters the tissue through a small or larger wound. When that happens, the body's immune system function kicks in. It attempts to stem the spread of bacteria. Immune cells then migrate towards the infected site and specifically attack the pathogens, keeping them from spreading to other healthy tissue. The immune cells utilise a membrane to isolate the infection, thereby creating a cavity. Pus – a semi-liquid mixture of bacteria, dead cells and dead tissue – then collects inside this cavity. Even though many people are disgusted by the thought of pus, it is basically the body's protective cleansing response to protect other healthy areas from infection.
What does an abscess look like?
One thing to keep in mind: Always seek medical advice as soon as you feel pressure pain in your mouth. We do not recommend self-diagnosis and comparing your symptoms to what you can see online. Armchair doctors are unable to say for sure whether you are suffering from an abscess or something entirely different. So, do not be unsettled by the images or talked into trying out some DIY treatment strategy, but seek the professional advice of a doctor, who can substantiate your suspicions.
Nevertheless, many people sit at home and ask themselves: What does an abscess look like? Generally speaking, a white "head" that resembles a spot may appear. This white fluid is the aforesaid collection of pus. Important to know: Deeper abscesses are often not readily visible. Your doctor will be able to say whether it really is an abscess or perhaps a harmless aphthae or simply a small oral sore.
Where can oral abscesses form?
Abscesses may form at various sites in the mouth. We have summarised the areas that tend to be more susceptible to abscesses and listed the different types of oral abscesses below:
- Inside of the cheeks
- Above the palate (palatal abscesses)
- In and below the lower jaw (perimandibular or submandibular abscesses)
- Below the tongue (sublingual abscesses)
- In inflamed gum pockets (parodontal abscesses)
- At the inflamed root tip of a tooth (apical abscesses)
- At the canine fossa in the facial skeleton (canine fossa abscesses)
Causes: Why do oral abscesses form?
An abscess usually forms as a result of external injuries, tissue damage or complications after surgery. The oral cavity is, unfortunately, a popular place for abscesses to form. This is due to the fact that it is home to a lot of bacteria. If there is any dental or mucous membrane damage, bacteria can swiftly penetrate deep into the tissue. Easy access is provided, for example, by:
- Periodontitis (inflammation of the periodontium)
- Inflammation of the pulp
- Injuries (e.g. bite marks on the inside of cheeks, mucosa wounds)
- Impacted wisdom teeth that do not have enough room to come in
- Injury after surgery to fit an implant (very rarely)
In general, people with a weakened immune system are more susceptible to developing an abscess – this is true, for example, for individuals infected with HIV/AIDS or taking immunosuppressants. The major risk groups also include diabetics with poorly controlled blood sugar levels.
Good to know:
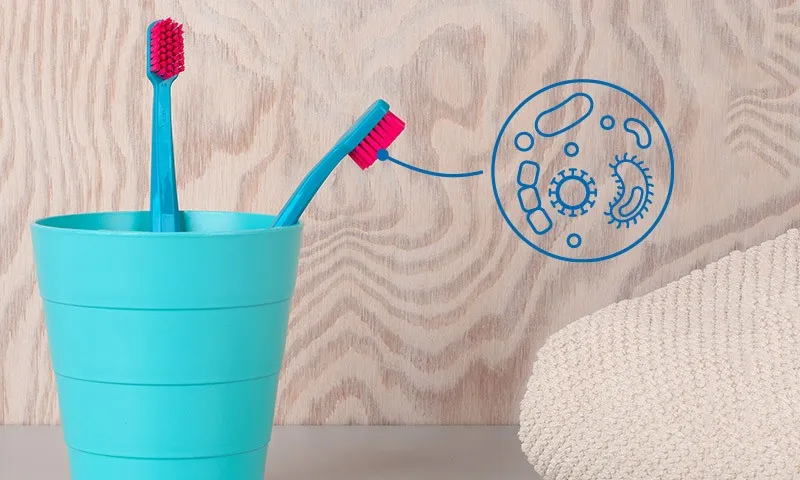
People who tend to neglect their oral hygiene have a higher risk of getting an abscess. Make sure to brush your teeth at least twice a day. What is the best way to do this? Simply read our tooth brushing instructions for optimum results.
However, it is also crucial to not only clean the easily accessible tooth surfaces but also the spaces between your teeth. That is best done using interdental brushes, which gently yet effectively remove bacteria and any food debris.
What are the symptoms of an oral abscess?
An oral abscess can manifest in many different ways; and there is no standard course of the condition. So, you should always be alert to any unpleasant changes in your oral cavity. That said, there are some symptoms that are commonly reported among abscess patients. We have summarised them below:
- Redness, swelling and warmth in the affected area
- Swelling around the cheek
- Toothache and/or jaw pain
- A chill and/or a high temperature
- A loose tooth (if the tooth is affected)
- Headache
- Swollen lymph nodes in the affected area of the neck
- Trouble swallowing
- Difficulty opening the mouth (in case of lower jaw abscesses)
- Bursting/leaking abscess with pus discharge
Caution: Some abscesses may be painless. So, always pay close attention to any changes in your mouth.
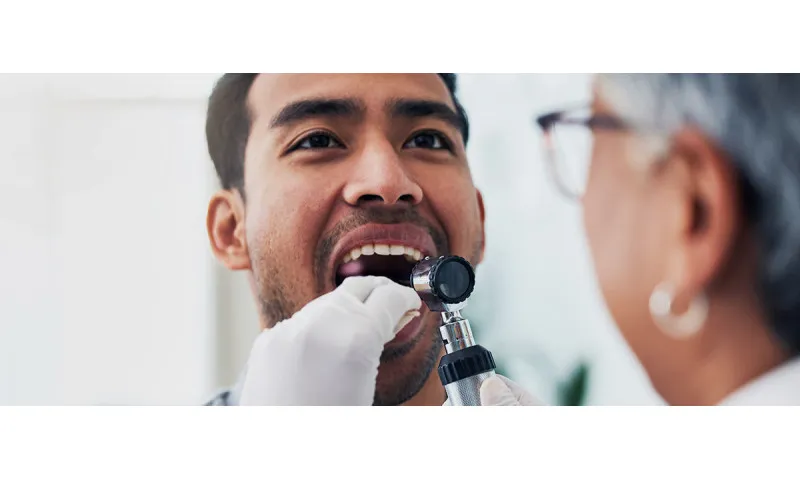
Oral abscess diagnosis
Oral abscesses are dangerous. If you have even the slightest suspicion, go and see a doctor immediately. Which health care professional should you see? Your family doctor, dentist or an ENT specialist should be your first point of contact.
The good news: If the abscess is detected at an early stage, it is usually quite easy to treat. What are the usual tests a doctor employs to diagnose an abscess? Quite often a visual examination is enough for a health care professional to recognise an oral abscess. As described above, sometimes a small white (pus-filled) spot can be seen, while other times only red swelling is visible. Together with the accompanying symptoms described by the patient – e.g. tenderness or even a high temperature – the doctor is able to make a diagnosis.
To be on the safe side, the doctor can also open and release some of the contents of the swelling. A blood count can also be performed to provide additional information about inflammation in the body. These diagnostic methods also help to detect any hidden abscesses.
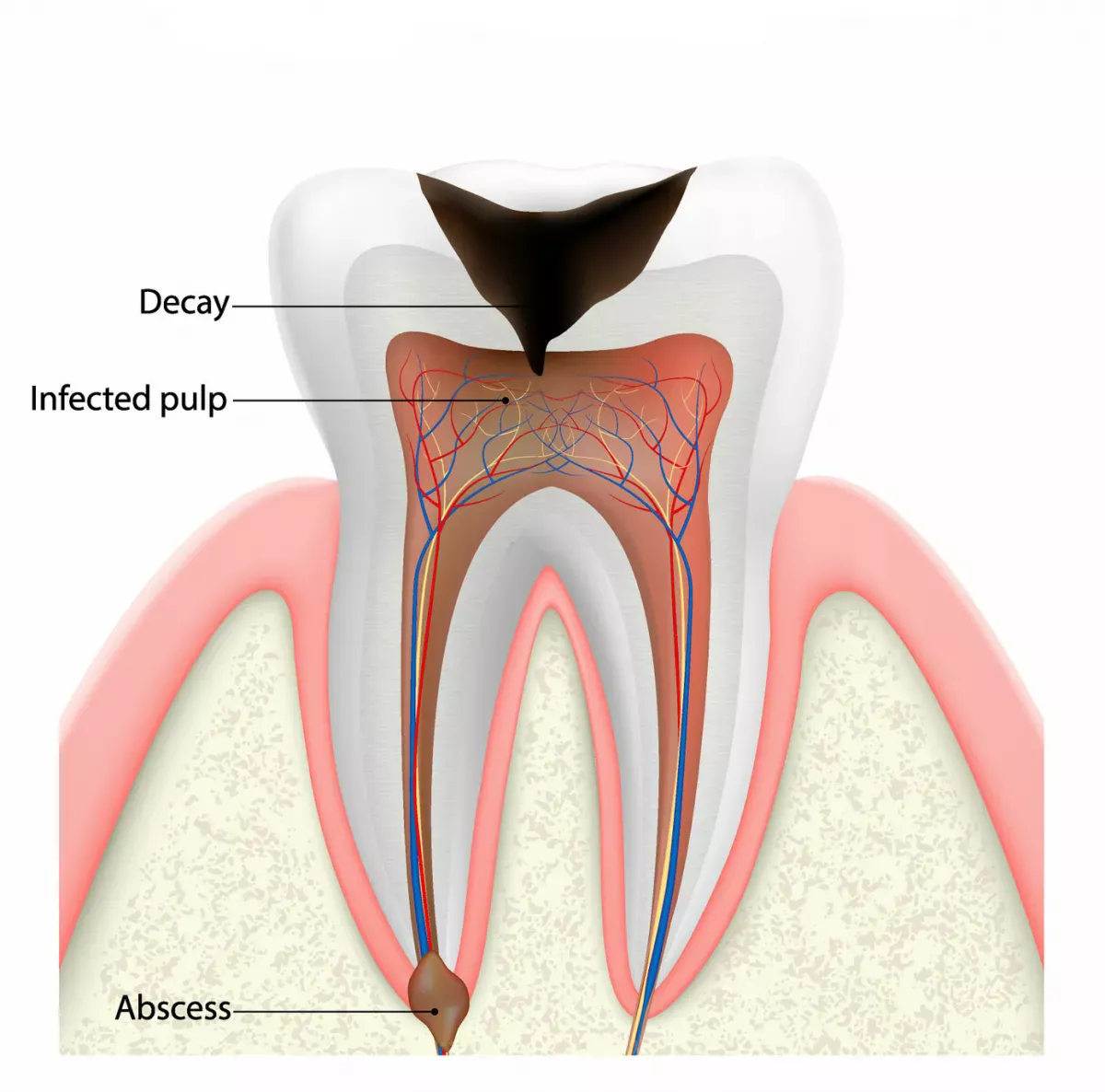
Dental abscess: What is that? How is it detected?
As described above, various types of abscesses can form in the oral cavity; including so-called dental abscesses. Needless to say, these dental abscesses are not actually located in the tooth, but in its immediate vicinity – as a pus-filled blister at the root tip, or apex, in the gums. In severe cases, the abscess can extend into the gums, cheeks or jaw bones.
Good to know:
An oral abscess is not to be confused with a dental fistula.
To detect such abscesses, a dentist can take an X-ray image, a computed tomography (CT) scan or a magnetic resonance imaging (MRI) scan. This also helps to determine how far the inflammation has spread.
What abscess treatment methods do dental practitioners recommend? The health care professional in charge of your treatment will provide all the information you need. In more severe cases, root canal treatment or root-end surgery may be necessary. Moreover, a root-treated tooth is, unfortunately, more susceptible to the formation of an abscess. Pus can also collect at the root tip of the dead tooth. Usually, the tooth then becomes increasingly sensitive to gentle tapping with a dental instrument. In other words, the dentist performs a "tapping test". A healthy tooth will not be tender to tapping, while an unhealthy one may experience a short, sharp, shooting pain – even after a very gentle tap – if there is inflammation present. Patients often also complain about feeling pressure pain in the mouth, teeth and jaw.
Abscess in a child's milk tooth
An abscess can also form in a child's mouth and is in fact more common than you might think. One reason for this: The enamel coating on a milk tooth is only about half as thick as that on adult teeth. As such, milk teeth are more susceptible to caries. This is because tooth enamel actually acts as a kind of hard protective barrier that helps prevent decay by keeping bacteria away from the tooth. The thinner enamel on milk teeth obviously provides less protection. Caries can then quickly work its way into the pulp and up to the tooth nerve.
In more acute cases, a dangerous abscess can form. Important to know: Caries, or dental decay, often strikes during childhood, as lots of children do not pay enough attention to their oral hygiene – so, at the end of the day, it is the responsibility of parents to make sure children brush their teeth correctly.
Brushing children's teeth correctly
If an abscess occurs in a milk tooth, it may be necessary to remove the affected tooth. And, as with adults, the pus also has to be drained. Your doctor will explain the exact treatment for an abscess in a milk tooth to you. If you think your child has an abscess, take them to see a health care professional right away!
Good to know:
As you have just learned, the best way to prevent the risk of abscess formation in the milk teeth is good oral hygiene. The CS Smart children's toothbrush from Curaprox makes brushing your child's teeth not only fun but also highly effective. The many individual filaments help remove plaque and food debris reliably. Thanks to its extra small head, this children's toothbrush is able to reach every corner of your child's mouth.
Therapy options: What to do about oral abscesses?
Since every patient is unique, no two treatments are exactly the same. Nevertheless, it can be said that draining the pus is key to healing. If that does not happen, there is a risk of the highly infectious mixture spreading throughout the body and causing immense damage; this happens, for example, if the abscess has burst and the collection of pus spreads into the surrounding tissue.
To prevent this happening, the health care professional will open and release the contents of the abscess under local anaesthetic. In some cases, drainage may require packing or a tube to keep the wound open to enable continued drainage. Without this packing or tube, the body would try to close the incision prematurely. Many patients ask themselves, when does an abscess really need to be incised and drained. Unfortunately, there is no general answer to this question. Your doctor will discuss the various options with you.
If everything goes to plan, the symptoms should subside within a few days. In the case of larger abscesses, where, for example, the symptoms include a high temperature and difficulty swallowing and breathing, the patient often has to be admitted to hospital immediately – which sometimes comes as great shock to the person affected, who does not consider their own situation to be so dramatic. The patient is then typically given intravenous antibiotics; and of course, in this case too, the abscess is immediately incised and drained. Sometimes a general anaesthetic is necessary for this procedure.
Once the acute infection has been treated and the pus drained, follow-up treatment may be essential. For example, in the case of a dental abscess, it might be necessary to remove the tooth that caused the abscess.
Home remedies for oral abscesses? No experiments, go and see a doctor right away!
Many people wish they could treat the bacterial infection naturally using some home remedies. Applying an ointment purchased at a pharmacy or gargling a bit with tea? Even if you have the feeling that these DIY treatments are helping to alleviate your symptoms, you must go and see a health care professional immediately if you have the slightest suspicion that you might be suffering from an abscess.
Purulent inflammation will not disappear on its own and will not be overcome with home remedies. The longer you wait, the worse the consequences can be. Only your doctor is able to decide whether an ointment can actually help as a supplement to your treatment. Sometimes, for example, a special drawing ointment is prescribed to drain the pus from the abscess cavity.
Do you want to treat an abscess with homoeopathic remedies? We advise you very strongly against doing this. Even if patients online tell of their successful healing journeys: Remember there is no scientific evidence that globules and the like actually work; any improvement is most likely down to a 'placebo' effect. However, this is not really going to help if pus is leaking from the abscess and spreading into the surrounding tissue.
And another important fact: Never try to open an abscess yourself. Do not attempt to squeeze or prick an abscess, as it could burst inwards releasing a purulent discharge into the body. If the abscess 'bursts' in this manner, the highly infectious mixture can enter the bloodstream unrestricted.
Just leave the painful and tender area alone and go and see a doctor to have it checked out professionally.
And then? Tips for a good healing process
Have you got over the initial shock and has the abscess in your mouth been treated successfully? Excellent! Nevertheless, you should follow a few essential tips over the coming days to ensure a good healing process. Read on to learn what you can do:
Relax as much as possible and avoid any strenuous activity
The incision and drainage of an abscess – whether under local or general anaesthetic – is a surgical procedure that should not be taken lightly. In the days following surgery, avoid sports and other leisure activities that involve a lot of physical movement. Going to the sauna and sunbathing are also out of the question. Your doctor will let you know when going back into the sun is safe. They will also give you some idea of how long you will be off sick and whether you will be provided with a sick note.
Do not neglect your oral hygiene practices
After oral surgery, your mouth will probably be sore and tender and you would most likely prefer to leave it alone. That is understandable. However, neglecting your dental care routine is not a good idea. If possible, continue to brush your teeth twice a day with a very soft toothbrush to prevent any infection taking hold. Obviously, you can and should avoid the sore and tender area. If you are unable to use a toothbrush at first, rinse your teeth with an antiseptic mouthwash prescribed by your dentist. But do not overdo it. Remember to spit out the mouthwash carefully, as it can otherwise put direct pressure on the wound.
Good to know:
You had an oral abscess and now have to resort to using a mouthwash instead of brushing your teeth for a few days: Perioplus+ Regenerate from Curaprox helps to actively speed up the healing process. The hyaluronic acid contained therein promotes cell growth and regeneration after surgery. And the chlorhexadine helps keep any bacteria at bay.
But again: Before using a mouthwash for the first time, ask your dentist which one is most suitable for your after-care treatment.
Are you looking for a toothbrush that will be particularly gentle on your teeth and gums after surgery? Then give the CS Surgical Mega Soft a try. It was developed precisely for this sensitive postoperative phase.
Avoid smoking and drinking alcohol
Obviously, it would be best to do this forever! But at least do it for three days after having an abscess incised and drained. Smoking and drinking alcohol can severely disrupt the healing process. Further, there might be some negative side effects when taking medication.
Be careful what you eat
After surgery, there will be a wound in your mouth. To avoid irritating the area, you should avoid eating hard and crunchy foods and stick to more liquid-based dishes, such as soups or porridge. This also reduces the likelihood of food debris entering the wound and causing an infection. Also avoid eating dairy products, as milk proteins can stick to the wound and the lactic acid bacteria can increase the risk of infection.
Food products that promote wound healing are ideal. These include mashed vegetable dishes made from potatoes or sweet potatoes and generally vegetables with a high vitamin A and C content, alongside vegetable oils rich in vitamin E, such as wheat germ and maize germ oil.
You might ask yourself: How long does the healing process take? Unfortunately, there is no standard answer to this question. If you are compliant and follow the aforesaid tips, there should be little in the way of a speedy recovery. However, it is essential to follow your doctor's orders carefully and to take follow-up appointments very seriously and not to miss them.
Summary: Abscesses are dangerous – go and see a doctor at the slightest suspicion
You have now learned that an abscess is not some harmless condition that will magically disappear all by itself. If you have the slightest suspicion that an abscess has formed in your mouth (or anywhere else in your body), go and see a health care professional right away. Never prod, poke or squeeze the affected area yourself, it will only make things worse.
It is impossible to make a general statement about the treatment your doctor will recommend. However, the abscess will usually need to be incised and drained. This is absolutely essential with an abscess, as there is otherwise a risk of the highly infectious mixture spreading throughout the body and causing immense damage.
The best way to prevent oral abscesses is good oral hygiene. Use your toothbrush to remove plaque and food debris from your teeth at least twice a day and also employ interdental brushes daily to clean the spaces between your teeth.
Sources:
Bundesverband für Ambulantes Operieren e.V.: Abszessspaltung.
Charité HNO-Klinik: Empfehlung zum Verhalten nach Mandelentfernung (Tonsillektomie).
Dr. med. dent. Dobbertin, Thomas: Aufklärung zur Eröffnung von intraoralen Abszessen.
Fair doctors: Zahnabszess: Symptome und Behandlung beim Zahnarzt, at: https://fair-doctors.de.
Dr. Lampmann, Martin: Entzündungen und Abszesse – harmlos, aber schmerzhaft, at: https://www.oralchirurgie-wallgraben.de/, updated: September 2016.
Dr. Schlotmann, Luca: Abszess im Mund at: https://www.dr-schlotmann.de/.
Dr. Dr. Scheerer, Friedrich: Entfernung von Abszessen im Mundraum at: https://mkg-wuppertal.de/.
Dr. med. dent. Seidel, Frank: Abszess, at: www.zahnarzt-drseidel.de.
Dr. Walensi, Mikolaj: OP-Anleitung Abszessentfernung - Raus mit dem eitrigen Graus, updated: 27/11/2014.
Van Waes, Hubertus J. M. et al.: Abszessbehandlung im Milchgebiss in: Farbatlanten der Zahnmedizin: Kinderzahnmedizin, updated: 2001.
All websites last accessed on 19 July 2023.
 Swiss premium oral care
Swiss premium oral care