Short overview
- Laryngeal cancer is mainly caused by smoking tobacco and drinking alcohol.
- This type of cancer is more common among men than women. It is very rare in children and young people. The first sign of the disease can be changes to the sound of your voice, such as hoarseness. Initially, laryngeal cancer symptoms might resemble common throat inflammation, leading to the disease often not being recognised at an early stage.
- If a malignant tumour in the larynx is detected early on, it can greatly enhance the chances of a full recovery, particularly if it has not yet spread to the lymph nodes. The prognosis becomes less favourable if the cancer is diagnosed late.
Laryngeal cancer: What is it actually?
The medical term for laryngeal or throat cancer is laryngeal carcinoma. The word "larynx" originates from the ancient Greek term for "upper windpipe". The word "carcinoma" is a more commonly recognised term: This term comes from the ancient Greek "karkinos", which literally translates as crab, or cancer in Latin.
Smoking and alcohol consumption are considered major risk factors for developing laryngeal cancer. Unfortunately, this malignant form of cancer is difficult to diagnose: The first signs and symptoms can resemble common inflammations. This is why doctors and patients do not always immediately associate these signs and symptoms with cancer, resulting in a delayed diagnosis and potentially damaging the prospects of recovery. This is particularly tragic because preliminary and early stages of laryngeal cancer can often be effectively treated with minimally invasive surgery.
A major indicator of possible laryngeal cancer is hoarseness, but also difficulty swallowing. This is especially true for smokers. If these symptoms persist for more than two weeks, it is crucial to go and have things checked by a health care professional.
Frequency: Men are affected significantly more frequently
Malignant tumours of the larynx rank third among the most common types of cancer that start in the head and neck region, following oral squamous cell and pharyngeal carcinomas. However, tumours in the head and neck region occur quite rarely overall.
Laryngeal cancer mainly affects men. The malignant tumour occurs seven times more frequently in males than in females. More precisely: In Germany, approximately 3,600 cases of laryngeal cancer are diagnosed annually in men, and about 500 in women. Based on statistical data, the affected individuals typically range between 50 and 70 years of age.
Laryngeal cancer is very rare in children and young people, with less than ten cases diagnosed in Germany each year.
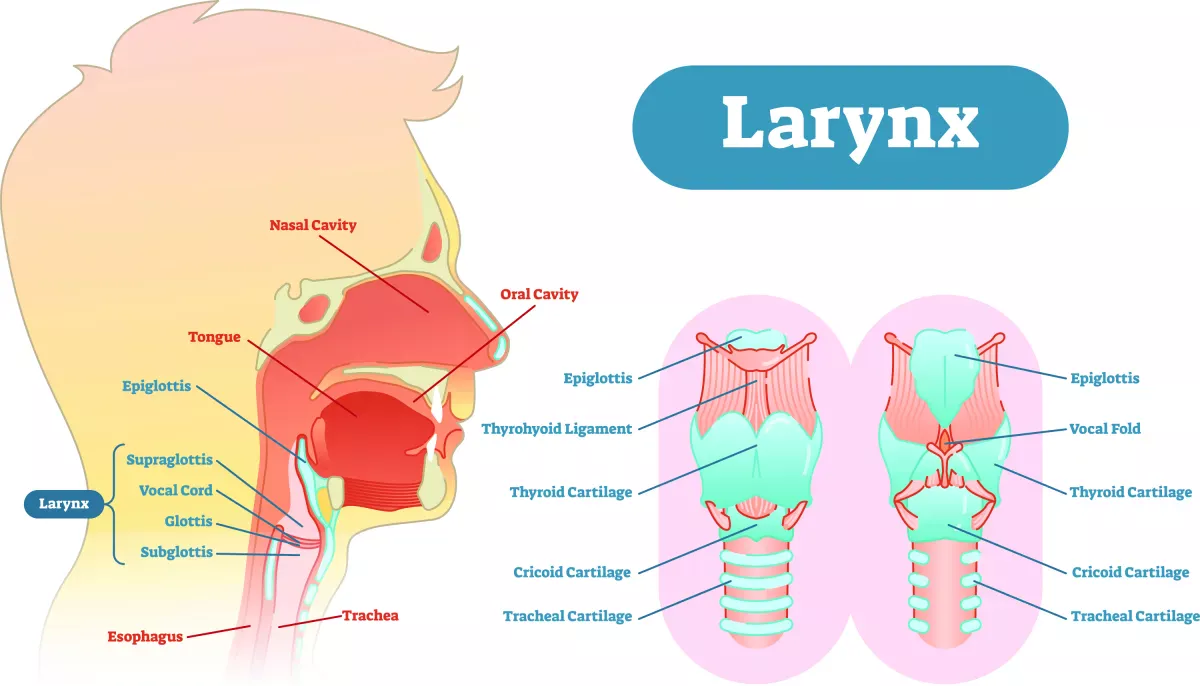
A look at the anatomy: This is how the larynx works
In order to understand laryngeal cancer properly, we need to take a brief look at the larynx and its tasks:
You can feel your larynx by gently placing a hand on the outside of your throat. Nevertheless, it is an organ not easily recognisable by most – unlike the heart or lungs, for instance. The following images can aid in understanding the anatomy of the larynx.
The larynx forms the upper end of the windpipe (trachea). Its function is to separate the air and food passages. This prevents food or foreign bodies from entering the windpipe. Moreover, the larynx functions as a voice box for producing sounds.
The larynx is made up of cartilage, which you can easily feel if you touch your throat. The thyroid and cricoid cartilages are easily discernible by touching.
Laryngeal cancer develops on the mucosa of the larynx, which is divided into three distinct areas:
- Supraglottis (area of the larynx above the vocal cords)
- Glottis (vocal cords)
- Subglottis (area below the vocal cords)
A malignant tumour of the larynx can develop on the mucosa of any of these three areas. Depending on its location, the tumour is termed:
- Supraglottic carcinoma (above the level of the vocal cords)
- Glottic carcinoma/vocal cord carcinoma (on the level of the vocal cords)
- Subglottic carcinoma (below the level of the vocal cords)
The most common site for tumours to develop is in the glottis. The least common site for tumours to develop is in the subglottis.
Causes and risk factors: Smoking poses the greatest risk
How does laryngeal cancer develop? We have summarised the risk factors for you below. The good news: You can actively protect yourself against the majority of them.
Smoking cigarettes and drinking alcohol
Smokers have the greatest risk of developing laryngeal cancer. However, regular alcohol consumption also significantly elevates the risk. The risk of developing laryngeal cancer in individuals who both smoke and drink is 30 times higher compared to non-smokers and non-drinkers.
Supraglottic carcinomas, occurring above the vocal cords, are notably associated with the influence of alcohol consumption. Smokers, on the other hand, are more predisposed to developing glottic carcinomas, which manifest as tumours on the level of the vocal cords.
Occupational risk factors
Individuals working with asbestos have a proven higher risk of developing laryngeal cancer. The disease is a recognised occupational disease in this case. This notably impacts professions such as construction workers, floor layers and roofers, among others.
Hereditary factors
There are documented familial clusters associated with laryngeal cancer. It is, therefore, assumed that laryngeal cancer also has a hereditary nature.
Weakened immune system
This explicitly does not refer to individuals who frequently experience a cold or cough. Rather, it pertains to those with HIV infections or patients who have undergone organ transplants and require immunosuppressants, thereby compromising their immune systems.
HPV infection
Infection with the human papillomavirus represents another risk factor, yet its significance in relation to laryngeal cancer is notably lower compared to tobacco and alcohol consumption. The virus can be transmitted through oral sex, for example. Fortunately, there is now a vaccine available to prevent HPV infections. In Germany, for instance, children aged nine and older have the option to receive immunisation against HPV.
Poor diet
A poor diet as a risk factor is subject to controversial discussions. However, a balanced diet, like the Mediterranean one, has demonstrated the potential to reduce the risk of developing laryngeal cancer by more than half. According to the guideline on laryngeal cancer by the Association of Scientific Medical Societies in Germany (Arbeitsgemeinschaft der Wissenschaftlichen Medizinischen Fachgesellschaften e. V., AWMF), special "key dietary components" include citrus fruits, fresh tomatoes, olive oil and fish oils. A high intake of polyunsaturated fatty acids is also linked to a reduced risk of laryngeal tumours.
What are the symptoms of laryngeal cancer?
As already mentioned, a tumour on the larynx can occur in different areas. Depending on its location, the tumour causes symptoms of varying severity. The symptoms of laryngeal cancer do not differ between men and women. Let us show and explain some characteristic signs to you below.
Possible symptoms of carcinomas in the supraglottis area (above the vocal cords):
- Difficulty swallowing
- Weight loss
- Pain that occasionally radiates towards the ears
- Sensation of a foreign body in the oral cavity
- Hoarseness (in the advanced stage)
Possible symptoms of carcinomas in the glottis area (vocal cords):
- Persistent hoarseness
- Scratchy throat
- Constant throat clearing
- Breathing difficulties and stridor (a high-pitched sound during inhalation) or shortness of breath (in advanced stages)
Good to know:
Tumours located in the glottis, i.e. the vocal cords, are often diagnosed early, leading to a more favourable prognosis. This is due to the fact that this type of tumour often prompts hoarseness even in the early stages, and individuals affected tend to seek medical attention.
Possible symptoms of carcinomas in the subglottis area (below the vocal cords):
- Breathing difficulties / shortness of breath
- Hoarseness
It is important to note that carcinomas in the subglottis area frequently go unnoticed for extended periods, with symptoms emerging typically as the tumour grows.
Important: If you are experiencing hoarseness or any of the aforementioned symptoms persistently for over two weeks, go and see an ENT specialist immediately. Tumours of the larynx that are detected early hold a high likelihood of successful treatment, particularly if they have not yet spread to the lymph nodes. By the way: In extreme cases, bad breath can also indicate laryngeal cancer. However, swelling of the neck is more commonly visible and palpable with laryngeal tumours. These are often lymph node metastases. In advanced stages, the tumour can protrude visibly from the outside when it invades through the laryngeal skeleton.
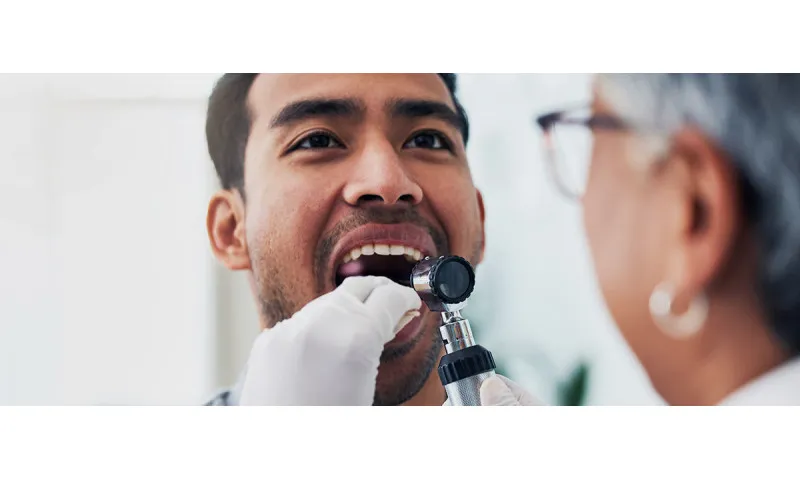
Diagnosis: How is laryngeal cancer diagnosed?
Many people wonder which specialist they should consult when suspecting laryngeal cancer. It is best to go and see an ENT specialist as soon as possible. Only an ENT specialist has the expertise and specialised equipment, like a laryngoscope, to examine the larynx thoroughly. They will also order a comprehensive series of additional tests and examinations. We have summarised them for you below.
Clinical examination
Your ENT specialist will begin by visually examining the accessible regions of your oral cavity and throat, then proceed to assess your nasopharynx, pharynx and larynx utilising mirrors and endoscopes. Typically, many patients anticipate that the diagnosis will involve a blood test. Yet, a blood count cannot definitively diagnose or exclude laryngeal cancer.
Panendoscopy
Following the clinical examination and a confirmed suspicion of laryngeal cancer, the most important procedure is the panendoscopy, which involves a thorough examination of the upper respiratory and digestive passages using endoscopes and a microscope. This examination is performed under general anaesthetic. During this procedure, the doctor can closely examine the mucosa and obtain small tissue samples for analysis by a pathologist. This type of examination enables an assessment of the tumour's size and its spread. The doctors can also rule out the presence of other tumours in the examined areas.
Ultrasound
Ultrasound can be used to determine whether the nearby lymph nodes of the neck are enlarged. Since enlarged lymph nodes may signify the spread of cancer to the lymph nodes – also termed lymphogenous metastasis.
Computed tomography (CT) scan
With the help of a computed tomography (CT) scan, the body can be X-rayed to create precise layered images, offering detailed visualisation. This imaging technique aids in diagnosing the spread of laryngeal cancer by determining the tumour's size, presence of lymph node metastases and distant metastases.
Magnetic resonance imaging (MRI) scan
A magnetic resonance imaging (MRI) scan can generate cross-sectional body images, particularly highlighting water and fatty tissue with high precision. The examination can be scheduled either in addition to the CT scan or instead of it. Typically, this decision is made by the doctor, often in collaboration with a multidisciplinary team, such as a tumour board.
Positron emission tomography (PET) scan plus CT
A positron emission tomography (PET) scan can help clarify ambiguous findings in the diagnosis. This type of diagnosis is usually ordered in conjunction with a CT scan (PET/CT). A PET/CT scan utilises the radionuclide glucose analogue fluorodeoxyglucose (FDG), a radioactive sugar. The underlying principle: Many tumours and metastases exhibit heightened sugar metabolism, which is detectable through FDG uptake in PET/CT scans. To conduct this procedure, the patient is injected with a minute quantity of the previously mentioned radionuclide. After an hour, a PET/CT scan is performed, revealing heightened sugar metabolism and aiding in locating potential metastases and tumours.
Good to know:
Many patients are understandably very afraid of metastases and ask themselves: Where does laryngeal cancer spread to? The most frequent site for metastases is in the cervical lymph nodes. When distant metastases form, they commonly manifest in the lungs and liver.
Classification systems and stages of laryngeal cancer
Tumours are categorised according to the TNM classification system. The ENT specialist uses this classification to determine the extent and stage of the tumour. In the TNM system, the overall stage is determined after the cancer has been assigned a letter to describe the tumour (T), node (N) and metastasis (M) categories.
Separate T categories with numbers are defined for each of the three areas of the larynx. The higher the T number, the larger the tumour and/or the more it has grown into nearby tissues: T1 and T2 describe smaller tumours. A stage T3 tumour already affects larger areas of the larynx but is still limited to this area. A stage T4 tumour has grown outside the larynx and into other body organs nearby:
- T4a: The tumour has grown outside the larynx and into structures nearby – for example into the thyroid cartilage, outer tongue muscles, thyroid gland, trachea and/or oesophagus.
- T4b: The tumour has grown outside the larynx and into vital organs – for example into the carotid artery or into regions that are no longer surgically accessible.
The description of the lymph nodes of the neck is similar. N0 means the cancer has not spread to nearby lymph nodes. Stages N1 to N3 describe the extent of cervical lymph node metastases.
The M stage is given as either M0 or M1. M0 means the cancer has not yet spread to distant parts of the body. M1 means the cancer has already spread to distant parts of the body.
The UICC stages of laryngeal cancer
The tumour classification system described above is further augmented by a staging system established by the UICC (Union for International Cancer Control). The respective UICC stage indicates the cancer's specific advancement or progression. The combination of both classification systems provides a complete picture of the severity and extent of laryngeal cancer.
According to the UICC, the stages are categorised as follows:
Stage 0
The tumour remains within the mucosal border (carcinoma in situ), the lymph nodes are not yet affected, there are no metastases (initial stage).
Stage 1
The tumour is small or only of medium size (corresponds to category T1). The lymph nodes are not yet affected, there are no distant metastases (also still initial stage).
Stage 2
Growth and spread are already advanced (corresponds to category T2), the lymph nodes are not yet affected, there are no distant metastases.
Stage 3
The size of the tumour can range from small to large (corresponds to categories T1 to T3), a lymph node is already affected, there are no distant metastases.
Stage 4a
This stage is reached when the tumour is either very large (T4a) or has extended into the cervical lymph nodes (N2).
Stage 4b
The tumour has grown outside the larynx and into important organs such as the carotid artery (corresponds to category T4b). Or: The patient has a metastasis in at least one cervical lymph node that is larger than six cm across or has spread to a lymph node and then grown outside of the lymph node (corresponds to category N3).
Stage 4c
In this final stage, distant metastases are present. This means that the tumour has already spread to other (distant) organs; in the case of laryngeal cancer, for example, this could be the lungs or liver. Usually, at this stage, there is no longer any prospect of a full recovery.
Life expectancy with laryngeal cancer
Statistically, in Germany, 62 percent of men and 65 percent of women with the disease are still alive five years after diagnosis. Important to know: These figures encompass all cases of laryngeal cancer. The actual life expectancy with laryngeal cancer heavily relies on the specific tumour stages outlined earlier. Patients in the early stages generally have a better life expectancy. Furthermore, glottic carcinomas (on the vocal cords) typically have the most favourable prognosis, while subglottic carcinomas (below the vocal cords) generally carry the least favourable prognosis.
Important: The individual prognosis always depends on the extent of tumour cell spread to the lymph nodes. Nine to twelve percent of patients experience tumour recurrences specifically in the region of the cervical lymph nodes. This often coincides with the occurrence of distant metastases and/or local recurrences at the original tumour site. Around 90 percent of these metastases and recurrences manifest within the initial two years following diagnosis.
The risk of developing another carcinoma in patients with malignant head and neck tumours is estimated to be between 10 and 20 percent. After five years without a tumour, patients are usually considered to be fully recovered.
So much for the statistics. While statistics provide guidance, individual journeys with cancer vary greatly. It is, therefore, crucial not to let these forecasts overshadow your own personal experience or hopes for the future. Instead, fostering a strong, open dialogue and trust with your doctor should take precedence over fixating on statistics and probabilities.
Types of treatment for laryngeal cancer
The treatment plan for laryngeal cancer is typically coordinated through multidisciplinary collaboration within a tumour board. This means that specialists from various fields such as otolaryngology, radiotherapy, oncology, pathology and radiology work together to collectively determine the most suitable type and method of treatment for the patient.
Surgery, radiotherapy and, if necessary, chemotherapy or immunotherapy are all treatment options for laryngeal cancer. In cases where a full recovery is possible, the goal of the treatment involves completely removing the tumour while preserving the voice and swallowing function to the greatest extent possible.
Find an overview of possible treatment approaches here.
Surgery
There are several ways to surgically remove a tumour from the larynx. The choice of surgery depends on the individual case, considering factors such as the size and location of the carcinoma within the larynx. The presence of cervical lymph node metastases also influences the choice of surgical approach.
Transoral surgery
Transoral surgery is a minimally invasive surgical technique that utilises a laser to remove tumours endoscopically through the mouth. The objective here is to conserve healthy portions of the larynx and to maintain its function to the greatest extent possible.
Transcervical surgery
If necessary, the surgeon removes the tumour from the outside, accessing it through the soft tissues of the neck. This approach is usually employed for larger tumours. Cervical lymph nodes must be removed from the outside, too. If feasible, the larynx can still be partially preserved during this procedure. It is also possible to remove the entire organ in this manner; this procedure is known as total laryngectomy and will be described in more detail in the next chapter.
Good to know:
Many patients wonder how long they will have to stay in hospital after surgery. Depending on whether the entire larynx or only a part of it had to be removed, the stay in hospital can vary between five and twelve days.
Radiotherapy
Radiotherapy alone may be considered as a treatment for laryngeal cancer, but typically only in special cases. Combined with chemotherapy, radiotherapy is a more commonly employed treatment approach. The tumour and the lymphatic drainage pathways in the neck are irradiated. Combining radiotherapy and chemotherapy reduces the risk of recurrence.
Even if the tumour has been operated on, additional radiotherapy might still be necessary. The former tumour region and the lymphatic drainage pathways are then irradiated.
Chemotherapy/immunotherapy
In certain cases, chemotherapy or immunotherapy may be considered for recurrences or distant metastases. Immunotherapies harness the body's immune system to combat cancer.
Alternative treatment
There is no known natural cure for throat cancer. The effectiveness of homoeopathic and home remedies has not yet been scientifically proven. Without the conventional medical treatments mentioned above, the course of the disease is fatal.
Total laryngectomy: Complete removal of the larynx
A total laryngectomy, which involves the complete removal of the larynx, becomes necessary when conservative methods like chemotherapy, radiotherapy or partial removal are no longer effective for advanced laryngeal tumours.
What happens when you have a total laryngectomy?
An ENT surgeon will perform a total laryngectomy in hospital under general anaesthetic. During the procedure, the surgeon removes all of your larynx. They may also remove some of your lymph nodes (neck dissection).
After a total laryngectomy, breathing and swallowing are completely separated. Next, your surgeon creates a so-called stoma (tracheostoma), which will help you breathe after surgery. From the outside, a hole is now visible in the neck, allowing you to breathe. Since: This hole leads directly to the windpipe, which the surgeon has sutured to the skin during surgery.
Talking in the normal way is no longer possible with a stoma. You will need a speech aid for this. It is also possible to learn a new speaking technique.
Even though these possibilities exist: The complete removal of the larynx typically represents a significant disruption to the lives of those affected. They often experience fears and worries. In such cases, seeking psychological support or connecting with other affected individuals and sharing your own experiences, whether through self-help groups or online forums, can be immensely beneficial in coping with the emotional challenges.
Life after total laryngectomy
Ideally, the laryngeal cancer has been completely removed after the procedure. In some cases, however, radiotherapy may still be required. As mentioned above, those affected are initially unable to talk after surgery. They have to learn a specific technique or use speech aids to communicate effectively. Unfortunately, there are additional restrictions that patients must adapt to in their daily lives:
- Loss of filtering through the airways
- Increased secretion
- Tickle in the throat
- Smell or sometimes taste disorders
- Restricted pushing when passing stool
Learning to talk with a tracheostoma
The primary concern for individuals without a larynx is usually to regain the ability to speak. We have summarised the options available here for you.
Learning the oesophageal substitute voice (ructus voice)
With the help of a speech therapist, those affected can learn to articulate sounds with the upper oesophageal muscle. This technique involves inhaling air into the oesophagus and subsequently expelling it using the abdominal muscles, resulting in a controlled release that is kind of like a "belch". Learning this substitute voice requires patience and lots of practice with the support of a speech therapist.
Tracheoesophageal puncture with voice prosthesis (shunt valve)
The voice prosthesis is usually inserted during the laryngectomy. To do so, the surgeon creates a passage, referred to as a fistula channel, between the rear wall of the trachea and the front wall of the oesophagus. This is where the voice valve prosthesis is inserted. Later on, the patient can generate sound by manipulating the opening in their neck or sealing the cannula. The sound is produced by pushing the exhaled air from your lungs through the voice prosthesis located in the fistula and up into your mouth. This air causes the top of the oesophagus to vibrate – producing a sound. Accompanying speech therapy is incredibly helpful in assisting individuals to learn this new method of speaking.
Electrolarynx
The electrolarynx is hardly used today. On the one hand, this is because the device is more cumbersome to use compared to other options, and, on the other hand, its resulting voice might sound strange or monotone, which can be off-putting for some individuals. Nevertheless, this option remains available and is thus presented here, too. The electrolarynx is a small device that patients hold against the softest possible part of their neck when they want to speak. The vibrating membrane of the device produces sounds. These sounds are transferred via the soft tissues of the neck into the oral cavity, allowing the patient to manipulate and shape them into speech.
Good to know:
If you are interested and want to know what the different laryngeal replacement voices sound like and how they differ, just take a look at sample videos on the Internet – for example on YouTube.
The right precautions
Laryngeal cancer is mainly caused by smoking. Therefore, not smoking is the best and most effective preventative measure against laryngeal cancer. As regular consumption of alcohol also increases the risk of developing malignant tumours of the larynx, it is advisable to stop drinking alcohol altogether or to minimise it as much as possible.
As smokers are high-risk patients, they should be regularly checked by an ENT specialist. An annual check-up is recommended from the age of 40. Individuals exposed to asbestos at work should also undergo regular check-ups.
Sources
AWMF online: Diagnostik, Therapie und Nachsorge des Larynxkarzinoms.
Bundeszentrale für gesundheitliche Aufklärung, at: www.impfen-info.de: HPV-Impfung bei Jugendlichen.
Bundesministerium für Bildung und Forschung: Immuntherapie – kann das Immunsystem Krebs bekämpfen?.
Deutsche Kinderkrebsstiftung, Tumoren des Rachens und Kehlkopfes.
Deutsche Krebsgesellschaft: Basisinfos für Patienten.
HNO-Ärzte im Netz: Kehlkopfkrebs: Jährliche Vorsorge und Früherkennung für Raucher wichtig.
Pflege.de: Tracheostoma.
Rudolf Probst, Gerhard Grevers, Heinrich Iro in: Hals-Nasen-Ohrenheilkunde (Thieme-Verlag), 3rd edition.
Schönweiler, Prof. Dr. med. Rainer, “Wie funktioniert eine Stimmprothese bzw. Shuntventil?”
Senner, Sonja Rosa Irmgard: Dissertation “Onkologische Ergebnisse fortgeschrittener Larynxkarzinome nach konservativer und operativer Therapie”, at: uni-muenchen.de.
Universitätsklinikum Erlangen: Informationsbroschüre für Patienten nach Laryngektomie.
Universitätsklinikum Düsseldorf: Panendoskopie.
Universitätsmedizin Mainz: Kehlkopf.
Universitätsmedizin Mannheim: Kehlkopfkrebs.
Uniklinik Köln: Wie läuft ein PET ab?.
All websites last accessed on 10 August 2023.
 Swiss premium oral care
Swiss premium oral care