Definition: What is floor of the mouth cancer?
Floor of the mouth cancer is a malignant tumour that forms on the oral mucosa between the lower jaw and the hyoid bone. The floor of the mouth is the lower boundary of the oral cavity located between the tongue and the lower jaw. As such, floor of the mouth cancer is a subtype of oral cavity cancer, belonging to the broader classification of head and neck tumours. The tumour spreads to neighbouring tissue and can, at an advanced stage, form metastases in the lymph nodes, potentially impacting other vital organs via the lymphatic system.
In around 90 percent of cases, floor of the mouth cancer is a squamous cell carcinoma. This means that the tumour is located on the uppermost layer of the oral mucosa. Adenocarcinomas, which usually evolve from the mucosal glands, are much rarer.
Floor of the mouth cancer is referred to in technical terms as squamous cell carcinoma of the floor of the mouth and is also abbreviated as floor of the mouth CA.
This article provides a basic overview of the symptoms, causes, prognosis and treatment of floor of the mouth cancer. For more information on oral cavity cancer in general, please refer to the main article "What to do about oral cavity cancer?".
Frequency of floor of the mouth cancer
Significantly more men are diagnosed with floor of the mouth cancer than women – around 75 percent of those affected are male. The majority of sufferers are aged between 55 and 70 years. According to estimates of the Robert Koch-Institut, roughly 12,000 people are diagnosed with oral cavity cancer in Germany each year; in about one tenth of these cases – i.e. around 1,200 people a year – the tumour is situated on the floor of the mouth.
The frequency of floor of the mouth cancer differs greatly around the world: For instance, in the USA, this type of cancer accounts for "only" five percent of all cancers; while in India, the figure is 50 percent. This is attributed to huge differences in oral hygiene and the tradition of betel chewing in India – the betel nut, in combination with slaked lime and betel leaves, has a stimulating and euphoric effect but is, unfortunately, carcinogenic.
Symptoms: Indication of floor of the mouth cancer
Early-stage floor of the mouth cancer is very difficult to identify, as it does not initially cause any symptoms. Most commonly, floor of the mouth cancer is indicated by a painless ulcer without defined borders that fails to heal.
Possible preliminary stages of floor of the mouth cancer
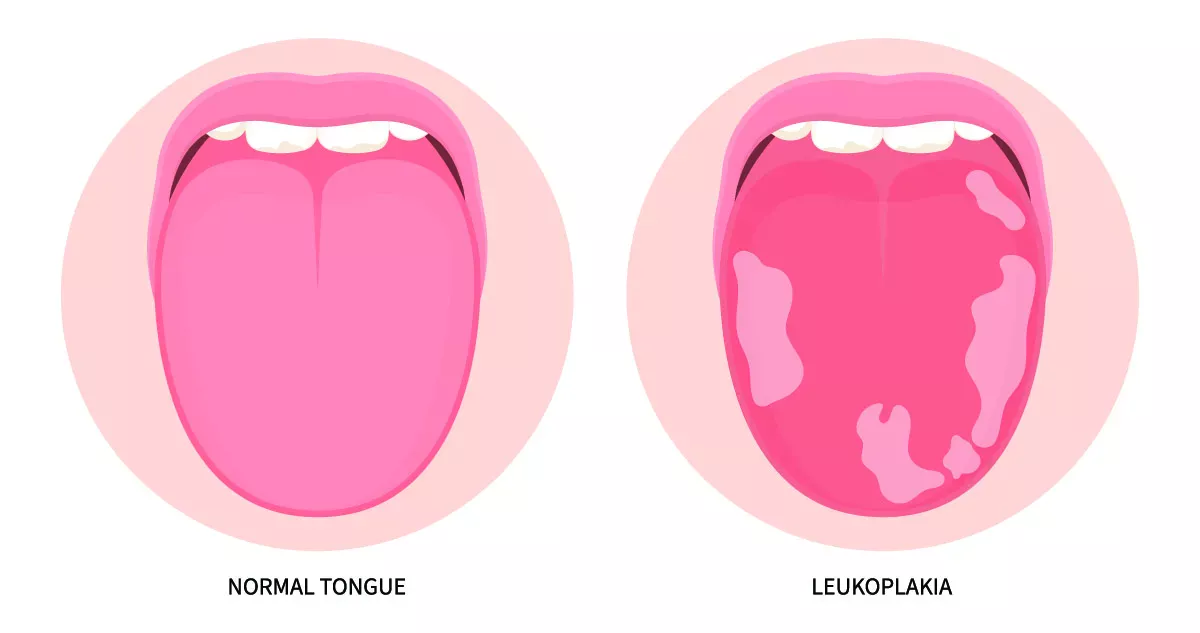
However, leukoplakia can also be an important warning sign. If left untreated, these white patches in the oral cavity can turn into a tumour. In 20 percent of the cases of floor of the mouth cancer, leukoplakia either coexists with or precedes tumour formation in nearby tissue.
If human papillomaviruses (HPV) are the trigger for floor of the mouth cancer, erythroplasia may also form. This is an isolated, deep-red lesion with a velvety surface that may indicate a tumour. Erythroplasia mainly occurs on the genitals but can also develop on the oral mucosa. Human papillomaviruses are typically linked to cervical cancer but can also be transmitted through oral sex, thus contributing to the development of floor of the mouth cancer.
Symptoms as the disease progresses
Besides an ulcer, the following symptoms may occur as floor of the mouth cancer progresses:
- Pain in the oral cavity that may sometimes spread to the nearest ear
- Bleeding (without any prior injury) at the affected area
- Bad breath
- Difficulty in eating, speaking and swallowing
- Swollen cervical lymph nodes
Additionally, symptoms of generally feeling unwell, e.g. tiredness, lethargy and loss of appetite.
What does floor of the mouth cancer look like?
The following images provide a rough idea of what floor of the mouth cancer actually looks like. Note, however, that every tumour appears different. If you detect a suspicious spot on the floor of your mouth, have it checked by a doctor to rule out floor of the mouth cancer – regardless of whether it is a lump, an ulcer, a white or red patch or a sore. Aphthae can also look very similar but typically resolve on their own after one to two weeks without the need for treatment. If the affected area fails to heal, it is best to go and see a health care professional.
Progression of floor of the mouth cancer
With floor of the mouth cancer, a distinction is made between two forms of progression:
Ulcerous form
About 99 percent of floor of the mouth tumours have an ulcerous form. This means that the tumour invades deep into existing tissue, leaving a "crater". The tumour grows extremely quickly and is often quite advanced by the time a diagnosis is made. Further, ulcerous tumours tend to develop into metastases. The prognosis for this form of the disease is, therefore, rather negative.
Verrucous form
In only about one per cent of all squamous cell carcinomas of the floor of the mouth does the tumour grow outwards at a gradual rate. This form of progression does not tend to lead to the development of metastases.
Causes: How does floor of the mouth cancer develop?
Floor of the mouth cancer occurs when cells with altered genetic information multiply and are not recognised by the immune system. These altered cancer cells gradually displace healthy cells and form a tumour, which grows either quickly or slowly depending on the type of tumour. When tumour cells migrate and settle in the lymph nodes, for example, doctors say the cancer has "metastasised". It is not yet known why this type of cell mutation occurs. However, there are a number of risk factors that increase the likelihood of developing floor of the mouth cancer.
Risk factors
The main risk factors for floor of the mouth cancer are:
- Drinking and smoking (also the use of "smokeless" tobacco products)
- Betel chewing (use of betel nuts; especially in Southeast Asia)
- Chronic inflammation due to poorly fitting dentures or sharp-edged teeth
- Virus infections (especially HPV)
- Untreated preliminary stages (e.g. leukoplakia)
- Poor oral hygiene
Diagnosis: Which health care professional should you see about floor of the mouth cancer?
If you have the slightest suspicion that you might be suffering from floor of the mouth cancer, consult your family doctor or an ENT specialist as early as possible. Since people with floor of the mouth cancer have no or only very minor symptoms at first, tumours are often only detected by chance during a routine dental check-up and clarification by an ENT specialist is recommended.
Which examination methods are used to diagnose floor of the mouth cancer?
A doctor will initially examine the affected area thoroughly and take a sample of tissue (biopsy) for analysis by a pathologist. This sample can be used to identify the presence of tumour cells and to establish the type of tumour.
If floor of the mouth cancer is confirmed, various imaging techniques are employed to assess how far the tumour has spread and whether metastases have already formed.
The following measures can be applied:
- Computed tomography (CT) scan
- Magnetic resonance imaging (MRI) scan
- Ultrasonic examination of the cervical lymph nodes
- X-ray examination of the lower jaw
A doctor determines which examinations are necessary.
Good to know:
More information on the diagnosis and classification of the tumour can be found in the main article on oral cavity cancer:
Treatment of floor of the mouth cancer
Treatment of floor of the mouth cancer may vary significantly depending on its location, size, form of progression and stage. It is not approved by just one doctor alone: Treatment usually takes place in a hospital, where specialists from various disciplines determine the most suitable way forward during regular multidisciplinary tumour conferences. The most common forms of treatment for squamous cell carcinomas of the floor of the mouth are presented below:
- Surgery
- Radiotherapy
- Chemotherapy
Various therapies can be used either alone or in combination, depending on individual needs. For example, radiotherapy might be sufficient to cure relatively small squamous cell carcinomas of the floor of the mouth. Otherwise, specialists often employ a combination of radiotherapy and chemotherapy.
If the tumour needs to be removed surgically, chemotherapy and/or radiotherapy treatment may be prescribed either before or after surgery. Doctors and patients have to carefully evaluate the advantages and disadvantages of action: Radiotherapy treatment often leads to severe side effects. For example, it may cause part of the jaw to die. Additionally, risk of the tumour recurring is slightly higher if additional radiotherapy is not performed on squamous cell carcinomas of the floor of the mouth. However, the final decision always lies with the patient.
Good to know:
Learn about the side effects of chemotherapy and radiotherapy treatment in the main article on oral cavity cancer:
Surgery for floor of the mouth cancer
During surgery for floor of the mouth cancer, the surgeon excises not only the tumour but also clinically healthy surrounding tissue with a margin of at least one centimetre to prevent invisible tumour cells from remaining in the floor of the mouth and forming a new tumour. If the cancer is already very advanced, it may be necessary to remove all or part of the lower jaw and tongue. If metastases have formed in the cervical lymph nodes or are suspected, they also have to be excised. This type of surgery is called a neck dissection.
Reconstruction after surgery for floor of the mouth cancer
If the jaw and tongue have been completely or partially removed during surgery to treat squamous cell carcinomas of the floor of the mouth, surgeons take your own tissue from another part of the body to restore function and aesthetics as much as possible. A surgeon can reconstruct the lower jaw and tongue by transplanting bone, for example, from the shoulder blade or fibula, along with tissue from the surrounding muscles and skin, and meticulously reconnecting blood vessels to those in the neck using microsurgery. This helps to ensure the circulation of blood. Depending on the individual circumstances of each case, several staged operations may be needed to perform reconstruction. Implants or well-fitting dentures can be used to enable proper chewing.
After-care and rehabilitation for floor of the mouth cancer
Treatment for squamous cell carcinomas of the floor of the mouth is usually followed by rehabilitation – also known as rehab. This type of care service is intended to prepare patients for a return to their everyday lives and can take place either in a specialised rehab clinic or on an outpatient basis.
If the jaw and tongue had to be completely or partially removed during surgery, it represents a deleterious effect on the patient’s quality of life. In some cases, basic bodily functions such as chewing, swallowing and speaking have to be relearned. Reconstructive surgery, coupled with bespoke speech therapy, aims to restore chewing and speech capabilities to the greatest extent possible. However, difficulties in swallowing and dry mouth may persist permanently.
Further, those affected should have regular check-ups to avoid any recurrence of their cancer. The intervals for these check-ups obviously vary from person to person.
Good to know:
Find out what you can do to alleviate persistent dry mouth in our article:
Prognosis: Life expectancy with floor of the mouth cancer
There is a good chance of recovery from floor of the mouth cancer. However, the prognosis depends significantly on how advanced the cancer is at the time of diagnosis: If the lymph nodes have not yet been affected, the average five-year survival rate is around 70 percent. However, if metastases have formed in the lymph nodes, the survival rate drops to about 20 to 25 percent. If distant metastases are found in critical organs or bones, life expectancy is, regrettably, much lower.
Preventative measures: How can you prevent floor of the mouth cancer?
Fortunately, there are certain things you can do to prevent the development of floor of the mouth cancer. To discover the main risk factors for cancer, German Cancer Aid (Deutsche Krebshilfe, DKH) is a good starting point. Every year during National Cancer Prevention Week, it takes a closer look at a specific risk factor. More information on general cancer prevention can be found on the website of the German Cancer Research Centre in the Helmholtz Association.
Quit drinking and smoking
Smoking tobacco and drinking alcohol on a regular basis can drastically increase your chances of developing oral cavity cancer. In fact, smokers who drink alcohol regularly are 30 times more likely to get oral cavity cancer and all other oral diseases. Your entire body will be truly grateful if you quit these harmful habits for good and adopt a healthier lifestyle.
Regular check-ups
Routine dental check-ups are important and highly recommended: On the one hand, your dentist can immediately recognise any abnormalities, thereby ensuring that floor of the mouth cancer is detected and treated as early as possible. On the other hand, they can determine permanent inflammation caused by sharp-edged teeth or ill-fitting dentures and suggest a suitable solution.
In addition to routine dental check-ups, self examine your own mouth regularly for any suspicious signs or changes. Discover how to do this in the article on oral cavity cancer.
Thorough oral hygiene
Poor oral hygiene also increases your risk of developing floor of the mouth cancer. Good dental hygiene includes the following routines:
- Brushing your teeth at least twice a day for three minutes each time, ideally in the morning after breakfast and at night before going to bed
- Cleaning your interdental spaces daily with interdental brushes
- Cleaning your tongue daily with a tongue scraper
- The following articles explain the scientifically proven best techniques for each routine:
- Brushing teeth correctly
- Cleaning interdental spaces correctly
- Brushing teeth correctly with an electric toothbrush
- Using a tongue scraper correctly
Sources
American Association of Oral and Maxillofacial Surgeons, Mouth Cancer Foundation: Oral Cancer Self-Exam.
Cedar Sinai: Floor of Mouth Cancer.
Deutsche Krebshilfe: Krebs im Mund-Kiefer-Gesichtsbereich (Die blauen Ratgeber).
Gesundheitsinformation.de: Aphten.
Guneren, Ethem: Malignant Tumors of the Floor of the Mouth, at: emedicine.medscape.com.
Kreppel, Matthias et al.: Diagnostik und Therapie des oralen Plattenepithelkarzinoms, at: zwp-online.info.
Leitlinienprogramm Onkologie (Arbeitsgemeinschaft der Wissenschaftlichen Medizinischen Fachgesellschaften e. V. (AWMF), der Deutschen Krebsgesellschaft e. V. (DKG) und der Stiftung Deutsche Krebshilfe: Patientenleitlinie Mundhöhlenkrebs.
Nabieva, Naiba: Erythroplasie, at: flexikon.doccheck.com.
Mendenhall, William et al.: Oral Cavity Cancer, in: Clinical Radiation Oncology. 2012.
Mühlenkreiskliniken: Wenn aus dem Bein ein Kiefer wird.
Robert Koch-Institut: Zentrum für Krebsregisterdaten.
Römer, Gunnar: Mundbodenkarzinom, at: flexikon.doccheck.com.
St. Franziskus-Hospital: Erfahrungsbericht: Weiterleben nach Mundbodenkrebs.
Tumorregister München: ICD-10 Co4: Mundboden. Inzidenz und Mortalität.
Universitätsklinikum Düsseldorf: Mundhöhlenkarzinom.
Urweider, Nicole: Schlucken, essen und lachen nach Mundhöhlenkrebs, at: blog.hirslanden.ch.
Wolf, Elke: Wund im Mund, at: pharmazeutische-zeitung.de.
ZWP: Bösartiger Tumor am Mundboden und Unterkiefer, at: zwp-online.info.
Zentrum für Krebsregisterdaten im Robert Koch-Institut: Datenbankabfrage, at: krebsdaten.de.
 Swiss premium oral care
Swiss premium oral care